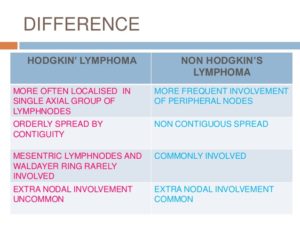
Treatments for both Hodgkin’s Lymphoma & Non-Hodgkin’s Lymphoma:
First the doctor needs to know what stage of cancer your in ranging from I to IV. This shows the doctor the following information to help the M.D. decide what treatment would be most effective to take.
- Stage I. The cancer is limited to one lymph node region or a group of nearby nodes or limited to a single organ.
- Stage II. In this stage, the cancer is in two lymph node regions, or the cancer has invaded one organ and the nearby lymph nodes as well. But the cancer is still limited to a section of the body either above or below the diaphragm.
- Stage III. When the cancer moves to lymph nodes both above and below the diaphragm, it’s considered stage III. Cancer may also be found in the lymph nodes above the diaphragm and in the spleen in non-Hodgkins and may also be in one portion of tissue or an organ near the lymph node groups or in the spleen in Hodgkins.
- Stage IV. This is the most advanced stage of non-Hodgkin’s and Hodgkin’s lymphoma. Cancer cells are in several portions of one or more organs and tissues.
- Stage III. When the cancer moves to lymph nodes both above and below the diaphragm, it’s considered stage III. Cancer may also be in one portion of tissue or an organ near the lymph node groups or in the spleen.
- Stage IV. This is the most advanced stage of Hodgkin’s lymphoma. Cancer cells are in several portions of one or more organs and tissues. Stage IV in both lymphomas affects not only the lymph nodes but also other parts of the body, such as the liver, lungs or bones.
Hodgkin Lymphoma Consultation
Your doctor will review your scans and discuss treatment options with you.
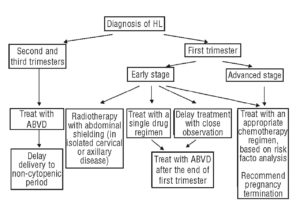
Which Hodgkin’s lymphoma treatments are right for you depends on the type and stage of your disease, your overall health, and your preferences. The goal of treatment is to destroy as many cancer cells as possible and bring the disease into remission.
Chemotherapy
Chemotherapy is a drug treatment that uses chemicals to kill lymphoma cells. Chemotherapy drugs travel through your bloodstream and can reach nearly all areas of your body.
Chemotherapy is often combined with radiation therapy in people with early-stage classical type Hodgkin’s lymphoma. Radiation therapy is typically done after chemotherapy. In advanced Hodgkin’s lymphoma, chemotherapy may be used alone or combined with radiation therapy.
Chemotherapy drugs can be taken in pill form or through a vein in your arm, or sometimes both methods of administration are used. Several combinations of chemotherapy drugs are used to treat Hodgkin’s lymphoma.
Side effects of chemotherapy depend on the drugs you’re given. Common side effects are nausea and hair loss. Serious long-term complications can occur, such as heart damage, lung damage, fertility problems and other cancers, such as leukemia.
Radiation therapy
Radiation therapy uses high-energy beams, such as X-rays and protons, to kill cancer cells. For classical Hodgkin’s lymphoma, radiation therapy is often used after chemotherapy. People with early-stage nodular lymphocyte-predominant Hodgkin’s lymphoma may undergo radiation therapy alone.
During radiation therapy, you lie on a table and a large machine moves around you, directing the energy beams to specific points on your body. Radiation can be aimed at affected lymph nodes and the nearby area of nodes where the disease might progress. The length of radiation treatment varies, depending on the stage of the disease. A typical treatment plan might have you going to the hospital or clinic five days a week for several weeks. At each visit, you undergo a 30-minute radiation treatment.
Radiation therapy can cause skin redness and hair loss at the site where the radiation is aimed. Many people experience fatigue during radiation therapy. More-serious risks include heart disease, stroke, thyroid problems, infertility and other cancers, such as breast or lung cancer.
Bone marrow transplant
Bone marrow transplant, also known as stem cell transplant, is a treatment to replace your diseased bone marrow with healthy stem cells that help you grow new bone marrow. A bone marrow transplant may be an option if Hodgkin’s lymphoma returns despite treatment.
During a bone marrow transplant, your own blood stem cells are removed, frozen and stored for later use. Next you receive high-dose chemotherapy and radiation therapy to destroy cancerous cells in your body. Finally your stem cells are thawed and injected into your body through your veins. The stem cells help build healthy bone marrow.
People who undergo bone marrow transplant may be at increased risk of infection.
Other drug therapy
Other drugs used to treat Hodgkin’s lymphoma include targeted drugs that focus on specific vulnerabilities in your cancer cells and immunotherapy that works to activate your own immune system to kill the lymphoma cells. If other treatments haven’t helped or if your Hodgkin’s lymphoma returns, your lymphoma cells may be analyzed in a laboratory to look for genetic mutations. Your doctor may recommend treatment with a drug that targets the particular mutations present in your lymphoma cells.
Targeted therapy is an active area of cancer research. New targeted therapy drugs are being studied in clinical trials.
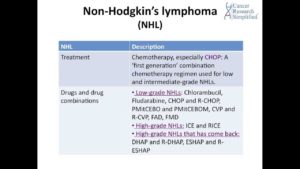
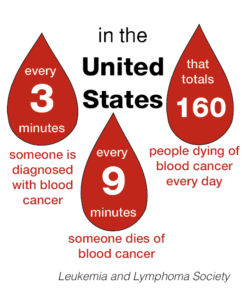
Now look at Non-Hodgkin’s Lymphoma Treatment and look at the similarities of Hodkin’s Lymphoma Rx; both are WBC’s Blood Cancers:
If your non-Hodgkin’s lymphoma is aggressive or causes signs and symptoms, your doctor may recommend treatment. Options may include:
Chemotherapy
Chemotherapy is a drug treatment — given orally or by injection — that kills cancer cells. Chemotherapy drugs can be given alone, in combination with other chemotherapy drugs or combined with other treatments.
Side effects of chemotherapy depend on the drugs you’re given. Common side effects are nausea and hair loss. Serious long-term complications can occur, such as heart damage, lung damage, fertility problems and other cancers, such as leukemia.
Radiation therapy
Radiation therapy uses high-powered energy beams, such as X-rays and protons, to kill cancer cells. During radiation therapy, you’re positioned on a table and a large machine directs radiation at precise points on your body. Radiation therapy can be used alone or in combination with other cancer treatments.
During radiation therapy, you lie on a table and a large machine moves around you, directing the energy beams to specific points on your body. Radiation can be aimed at affected lymph nodes and the nearby area of nodes where the disease might progress. The length of radiation treatment varies, depending on the stage of the disease. A typical treatment plan might have you going to the hospital or clinic five days a week for several weeks, where you undergo a 30-minute radiation treatment at each visit.
Radiation therapy can cause skin redness and hair loss at the site where the radiation is aimed. Many people experience fatigue during radiation therapy. More-serious risks include heart disease, stroke, thyroid problems, infertility, and other cancers, such as breast or lung cancer.
Bone marrow transplant
Bone marrow transplant, also known as a stem cell transplant, involves using high doses of chemotherapy and radiation to suppress your bone marrow. Then healthy bone marrow stem cells from your body or from a donor are infused into your blood where they travel to your bones and rebuild your bone marrow.
People who undergo bone marrow transplant may be at increased risk of infection.
Other drug therapy
Biological therapy drugs help your body’s immune system fight cancer.
For example, one biological therapy called rituximab (Rituxan) is a type of monoclonal antibody that attaches to B cells and makes them more visible to the immune system, which can then attack. Rituximab lowers the number of B cells, including your healthy B cells, but your body produces new healthy B cells to replace these. The cancerous B cells are less likely to recur.
Also, a drug called ibrutinib (Imbruvica) has been approved by the Food and Drug Administration (FDA) for some people undergoing treatment for non-Hodgkin’s lymphoma.
Radioimmunotherapy drugs are made of monoclonal antibodies that carry radioactive isotopes. This allows the antibody to attach to cancer cells and deliver radiation directly to the cells. An example of a radioimmunotherapy drug used to treat non-Hodgkin’s lymphoma is ibritumomab tiuxetan (Zevalin).
Clinical trials
Clinical research studies (clinical trials) may be an option for people whose disease has not been controlled by other treatment options. Ask your doctor about possible clinical trials for your type of non-Hodgkin’s lymphoma.