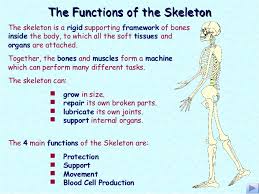


The infrastructure of the human body that allows us to perform our daily activities from standing, to sitting, to walking, or even climbing is our skeletal system. The major pillar or beam in the skeletal system is the vertebral column (spinal column). This bone structure allows us to bend, stand upright, twist, to dancing up a storm down the happy trail of life, if taken care of properly. If not, you may not be considering your life a happy tune, during that time of injury that can be a short or long haul before resolved, if ever. This infrastructure is so vital in our activities of our daily life. Many of us don’t realize that until the injury or damage sets in. There is one way you can bypass this disaster, don’t have it become a part of your life which is taking preventative measures; especially if you do heavy lifting in your life; like in my job as a nurse. One major ingredient to preventative measures is proper body mechanics but the trick here is never lift heavy items from below your waist level without bending your legs or even better without a second person helping you or some form of support but there is more to it than just that. There are more factors involved in helping you keep your back with all other bones strong. That would be healthy dieting, maintaining a good weight for your height (body mass index), and good exercise (not necessarily work out but if that is what you enjoy doing, it’s even better and don’t stop). All these ingredients to a better development and maintenance of your skeletal system=HEALTHY HABITS. A plus and benefit that many choose to do is going regularly to a chiropractor who can keep your spine in alignment (see one before injury starts). Recommended in Rockland County, NY is Dr. Diane Gregory, who I go to for my back and who has done both prevention & Rx; www.gregorychiropractic.com.
The key is to be living a healthy life. This consists of diet, exercise, activity and healthy habits learned and practiced in your routine of daily living that will help prevent or assist you in treating bone and back injuries; even problems caused by the inactivity with doing heavy lifting (Ex. lack of any muscle tone or muscle knots), which can inflict bone or back injuries. The better we treat ourselves EVERYDAY regarding health the higher the odds we will live a longer life. One common problem in America that can occur if not living healthy and/or using improper body mechanics with heavy lifting, especially frequently, can increase the risk of sciatica nerve damage. The pain of sciatica is typically felt from the low back (lumbar area) to behind the thigh and radiating down below the knee. The sciatica nerve is the largest nerve in the body that begins from nerve roots in the lumbar spinal cord in the low back and extends through the buttock to send the nerve ending down the lower limb to the foot. Depending on the precise cause of the sciatica symptoms with the duration, the outlook for recovery from sciatica ranges from excellent to having long term chronic symptoms. This can be prevented to some extent by avoiding low back trauma injuries. Thinking before lifting is the one of the best ideas. Osteoporosis is a common bone problem that is a abnormal loss of bony tissue resulting in fragile porous bones attributable to a lack of calcium, most common in postmenopausal women. This progressive bone disease that’s characterized by a decrease in bone mass and density leads to an increased risk of a fracture. The causes of this disease that are modifiable (can be changed) would be: Vitamin D deficiency, menopause, excess alcohol, tobacco smoking, malnutrition (identified risk factors include low dietary calcium and/or phosphorus, magnesium, zinc, boron, iron, fluoride, copper, vitamins A,K,E, and C; also D where skin exposure to sunlight provides an inadequate supply. Excess sodium is a risk factor. High blood acidity may be diet related, and is a known antagonist to the bone. Some have identified low protein intake as associated with lower peak bone mass during adolescence and lower bone mineral density in elderly populations. Other risk factors are inactive, underweight, heavy leads-a strong association between cadmium and lead with bone disease has been established. Low-level exposure to cadmium is associated with an increased loss of bone mineral density readily in both genders. Some studies even show soft drinks can increase the risk of osteoporosis related to high phosphoric acid. Others suggest soft drinks may displace calcium containing drinks from the diet rather than causing osteoporosis.
Another bone disorder is osteomalacia that is a softening of the bones caused by defective bone mineralization secondary to inadequate amounts of available phosphorus and calcium. The most common cause of the disease is a deficiency in vitamin D, which is normally obtained from the diet and/or from sunlight exposure. We can help our bones in many ways. There is not just one food to eat or one type of exercise to do or one healthy habit to practice to keep you healthy with strong bones, there are choices. Wouldn’t you want less risk of bone or back injury or disease for yourself and for others throughout the nation including the future generations? Than join me and others. If you like what you see spread the good cheer. Let’s build a stronger foundation regarding HEALTH in America.
Adults need 700mg of calcium a day. You should be able to get all the calcium you need by eating a varied and balanced diet.
Foods healthy for bones and Good sources of calcium include::
- milk, cheese and other dairy foods.
- green leafy vegetables, such as broccoli, cabbage and okra, but not spinach.
- soya beans.
- tofu.
- plant-based drinks (such as soya drink) with added calcium.
- nuts.
- bread and anything made with fortified flour.
- fish where you eat the bones, such as sardines and pilchards.