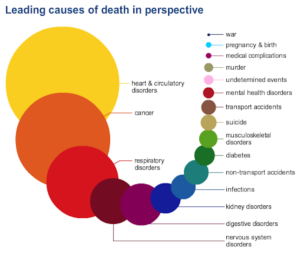
4: Stroke (cerebrovascular diseases)
- Deaths: 128,932
- Males: 52,335
- Females: 76,597
- Rate: 41.4
- Age-adjusted rate: 37.9
- Percentage of total deaths: 5.12%.
Cerebrovascular diseases are conditions that develop as a result of problems with the blood vessels that supply the brain. Four of the most common types of cerebrovascular disease are:
-
- Stroke
- Transient ischemic attack (TIA)
- Subarachnoid hemorrhage that highly leads into a stroke, depending on how quick the hemorrhage is detected with how bad of a hemorrhage it is When a pt comes in the ER and shows symptoms of a TIA or stroke the first thing the MD does within 10 minutes by law is order a CT of the head to see if its a clot or a hemorrhage in the brain that is causing the stroke or TIA to decide his or her pathway of treatment. It would tell the MD decide whether to decide as surgery for a hemorrhage or if a clot start rTPA a con- tinuous IV infusion to treat the clot if the stroke symptoms started in the past 6 (using a vein) or to 8 hours (using an artery) or another treatment would be decided if it was a clot with s/s that past.
Every year more than 795,000 people in the US have a stroke; risk of having a stroke varies with race, ethnicity, age and geography. Risk of stroke increases with age, yet in 2009 34% of people hospitalized for stroke were younger than 65 years.
The highest death rates from stroke in the US occur in the southeast.
Major warning signs and symptoms of stroke
During a stroke, every second counts. Fast treatment can reduce the brain damage that stroke can cause.
Signs and symptoms of stroke include sudden:13
- Numbness or weakness in the face, arm or leg, especially on one side of the body
- Confusion, trouble speaking or difficulty understanding speech
- Trouble seeing in one or both eyes
- Trouble walking, dizziness, loss of balance or lack of coordination
- Severe headache with no known cause.
Call 9-1-1 immediately if any of the above symptoms are experienced.
If you think someone may be having a stroke, act F.A.S.T. and do the following simple test:
- F – Face: ask the person to smile. Does one side of the face droop?
- A – Arms: ask the person to raise both arms. Does one arm drift downward?
- S – Speech: ask the person to repeat a simple phrase. Is their speech slurred or strange?
- T – Time: if you observe any of these signs, call 9-1-1 immediately.
Note the time when any symptoms first appear. Some treatments for stroke only work if given within the first 3 hours after symptoms appear.
Do not drive to the hospital or let someone else drive you. Call an ambulance so that medical personnel can begin life-saving treatment on the way to the emergency room.
How can stroke be prevented?
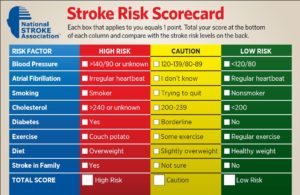
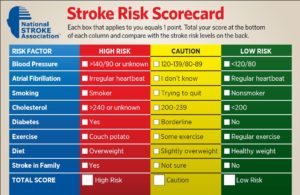
High blood pressure, high cholesterol, and smoking are major risk factors for stroke. About half of Americans (49%) have at least one of these three risk factors. Several other medical conditions and unhealthy lifestyle choices can increase your risk for stroke.
Although you cannot control all of your risk factors for stroke, you can take steps to prevent stroke and its complications.12
Stroke prevention measures may include:14,15
- Eating a healthy diet
- Maintaining a healthy weight
- Getting enough exercise
- Not smoking
- Limiting alcohol use
- Checking cholesterol
- Controlling blood pressure
- Managing diabetes
- Managing heart disease
- Taking medicine correctly
- Talking with a health care team.
Recent developments on stroke from MNT news:
Potassium-rich foods could lower stroke risk in older women
Researchers have found that older women whose diets involve potassium-rich foods may be at a reduced risk of stroke and have a greater life expectancy than women consuming less potassium-rich foods.
Stroke risk lowered with a high-protein diet
A diet higher in protein may reduce stroke risk by 20%, while every additional 20 grams of protein consumed each day could reduce stroke risk by 26%, according to new research.
5: Accidents (unintentional injuries)
- Deaths: 126,438
- Males: 79,257
- Females: 47,181
- Rate: 40.6
- Age-adjusted rate: 39.1
- Percentage of total deaths: 5.02%.
Accidents, also referred to as unintentional injuries, are at present the 5th leading cause of death in the US and the leading cause of death for those between the ages 1 to 44. The National Highway Traffic Safety Administration say that highway crashes alone have an annual price tag of around $871 billion in economic loss and social harm, with speeding accounting for $210 billion of that figure.
Data for accidents include the following:
- Motor vehicle accidents
- Other land transport accidents
- Water, air and space accidents
- Accidental discharge of firearms
- Accidental drowning and submersion
- Falls
- Accidental exposure to smoke, fire and flames
- Accidental poisoning and exposure to noxious substances.
Possible prevention measures
Accidents cause loss and suffering to the victims and their loved ones. Methods of safety and prevention can help toward avoiding some forms of unintentional death.
Seat belts have saved an estimated 255,000 lives between 1975 and 2008.
In 2010, 10,228 people were killed in alcohol-impaired driving crashes, accounting for nearly one-third (31%) of all traffic-related deaths in the US.1 In 2010, over 1.4 million drivers were arrested for driving under the influence of alcohol or narcotics.3 That is 1% of the 112 million self-reported episodes of alcohol-impaired driving among US adults each year.4
Information on saving lives and protecting people from violence and injuries can be found on the Centers for Disease Control and Prevention (CDC) website.
Some facts or statistics show:
Violence or injury ‘responsible for almost 80% of deaths in Americans under 30’
More Americans between the ages 1-30 die due to preventable causes such as car crashes, falls and firearm-related injuries, according to a new report.
How a smartphone could prevent falls
Purdue University researchers have created a smartphone tool – called SmartGait – that can measure a person’s walking gait, which they say could prevent falls.
6: Alzheimer’s disease
- Deaths: 84,974
- Males: 25,677
- Females: 59,297
- Rate: 27.3
- Age-adjusted rate: 24.7
- Percentage of total deaths: 3.37%.
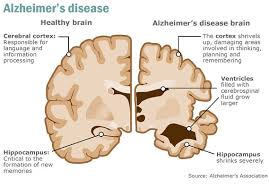
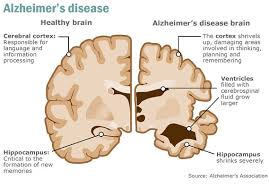
Dementia is an overall term for diseases and conditions characterized by a decline in memory or other thinking skills that affect a person’s ability to perform everyday activities. Dementia is caused by damage to nerve cells in the brain which are called neurons. As a result of the damage, neurons can no longer function normally and may die. This, in turn, can lead to changes in memory, behavior and the ability to think clearly.
Alzheimer’s is the sixth leading cause of death in the US with around 84,974 deaths each year.
For people with Alzheimer’s disease, the damage and death of neurons eventually impair the ability to carry out basic bodily functions such as walking and swallowing.
People in the final stages of the disease are bed-bound and require around-the-clock care. Alzheimer’s is ultimately fatal. Alzheimer’s disease accounts for 60-80% of dementia cases.
An estimated 5.2 million Americans may have Alzheimer’s disease in 2014, including approximately 200,000 individuals younger than age 65 who have younger-onset Alzheimer’s.
Almost two-thirds of American seniors living with Alzheimer’s are women. Of the 5 million people age 65 and older with Alzheimer’s in the US, 3.2 million are women, and 1.8 million are men.
In 2013, 15.5 million family and friends provided 17.7 billion hours of unpaid care to those with Alzheimer’s and other dementias – care valued at $220.2 billion, which is nearly eight times the total revenue of McDonald’s in 2012.
Alzheimer’s disease is one of the most expensive conditions in the nation. In 2014, the direct costs to American society of caring for those with Alzheimer’s will total an estimated $214 billion, including $150 billion in costs to Medicare and Medicaid. Despite these staggering figures, Alzheimer’s will cost an estimated $1.2 trillion (in today’s dollars) in 2050.
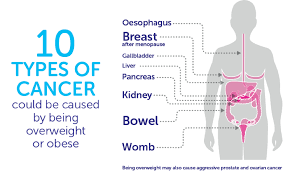
A woman’s estimated lifetime risk of developing Alzheimer’s at age 65 is 1 in 6, compared with nearly 1 in 11 for a man. As real a concern as breast cancer is to women’s health, women in their 60s are about twice as likely to develop Alzheimer’s during the rest of their lives as they are to develop breast cancer.
Warning signs and symptoms of Alzheimer’s disease
The following are common signs and symptoms of Alzheimer’s:
- Memory loss that disrupts daily life
- Challenges in planning or solving problems
- Difficulty completing familiar tasks at home, work or in leisure
- Confusion with time or place
- Trouble understanding visual images and spatial relationships
- New problems with words in speaking or writing
- Misplacing things and losing the ability to retrace steps
- Decreased or poor judgment
- Withdrawal from work or social activities
- Changes in mood and personality, including apathy and depression.
Can Alzheimer’s be prevented?
As the exact cause of Alzheimer’s disease is still unknown, there is no way to prevent the condition. However, there are some steps you can take that may help to delay the onset of dementia.26
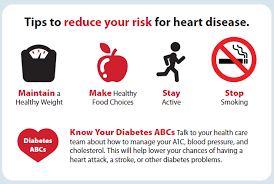
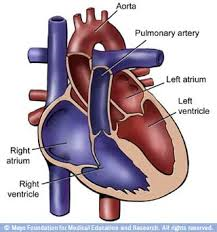
Reducing your risk of cardiovascular disease
Cardiovascular disease (disease of the heart or blood vessels) has been connected with an increased risk of Alzheimer’s disease and vascular dementia.
Risk of developing cardiovascular disease, as well as stroke and heart attacks, may be reduced by improving cardiovascular health using steps such as:
- Stopping smoking
- Avoiding large quantities of alcohol
- Eating a healthy balanced diet
- Exercising for at least 150 minutes (2 hours and 30 minutes) every week by doing moderate-intensity aerobic activity (such as cycling or fast walking), which improve both your physical and mental health
- Check blood pressure through regular health tests
- If you have diabetes, make sure you keep to the diet and take your medicine.
Staying mentally active
Evidence suggests rates of dementia are lower in mentally, physically and socially active people. It may be possible to reduce the risk of Alzheimer’s disease and other types of dementia by:
- Reading
- Writing for pleasure
- Learning foreign languages
- Playing musical instruments
- Taking part in adult education courses
- Playing tennis
- Playing golf
- Swimming
- Group sports, such as bowling
- Walking.
Future research
Other methods to treat or prevent Alzheimer’s may be revealed as research into the condition continues. At present, there is no evidence to support using the following to prevent dementia:
- Statins (cholesterol-lowering medicines)
- Hormone replacement therapy (when powerful chemicals are taken to replace those that your body no longer produces)
- Vitamin E (found in a variety of foods, such as olive oil, nuts and seeds)
- Non-steroidal anti-inflammatory drugs (NSAIDs).
Learn more about Alzheimer’s
Recent developments on Alzheimer’s from MNT news
Impaired brain signaling pathway ‘may be a cause of Alzheimer’s’
Mayo Clinic researchers say a brain signaling defect in the Wnt pathway may be a cause of Alzheimer’s, and boosting Wnt signaling could prevent the disease.
Alzheimer’s disease: are we close to finding a cure?
There seems to be more focus than ever on Alzheimer’s research. But how close are scientists to developing effective prevention and treatment strategies for the disease?