Measures for Prevention of Stomach (Gastric) Cancer Risk:
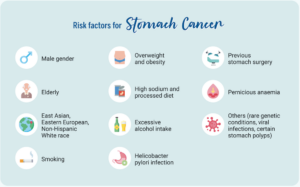
Smoking cessation
Based on solid evidence, smoking is associated with an increased risk of stomach cancer. The 2004 Surgeon General’s report identifies cigarette smoking as a cause of stomach cancer, with an average relative risk (RR) in former smokers of 1.2 and in current smokers of 1.6. Compared with persistent smokers, the risk of stomach cancer decreases among former smokers with time since cessation. This pattern of observations makes it reasonable to infer that cigarette smoking prevention or cessation would result in a decreased risk of gastric cancer.
H. pylori infection eradication
Based on solid evidence, H. pylori infection is associated with an increased risk of gastric cancer.
Treat stomach infections. If you have ulcers from an H. pylori infection, get treatment. Antibiotics can kill the bacteria, and other drugs will heal the sores in the lining of your stomach to cut your risk of cancer.
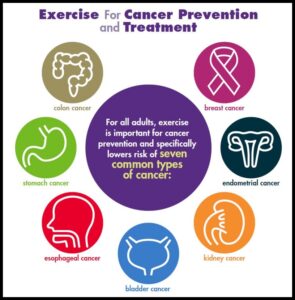
Diet
Eat healthy. Get more fresh fruits and vegetables on your plate every day. They’re high in fiber and in some vitamins that can lower your cancer risk. Avoid very salty, pickled, cured, or smoked foods like hot dogs, processed lunch meats, or smoked cheeses. Keep your weight at a healthy level, too. Being overweight or obese can also raise your risk of the disease.
Based on fair evidence, excessive salt intake and deficient dietary consumption of fresh fruits and vegetables are associated with an increased risk of gastric cancer. Dietary intake of vitamin C contained in vegetables, fruits, and other foods of plant origin is associated with a reduced risk of gastric cancer. Diets high in whole-grain cereals, carotenoids, allium compounds, and green tea are also associated with a reduced risk of this cancer. However, it is uncertain if changing one’s diet to include more vegetables, fruits, and whole grains would reduce the risk of gastric cancer.
TREATMENTS FOR STOMACH CANCER:
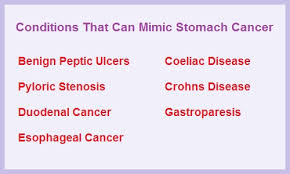
Many treatments can fight stomach cancer. The one you and your doctor choose will depend on how long you’ve had the disease or how much it has spread in your body, called the stage of your cancer.
Surgery. Your doctor might remove part of your stomach or other tissues nearby that have cancer cells. Surgery gets rid of the tumor and stops cancer from spreading to other parts of your body. If your disease is in a more advanced stage, your doctor might need to remove all of your stomach=Gastrectomy or in some other cases the Surgeon may only have to remove part of the stomach=Partial Gastrectomy.
Some tumors can keep food from moving in and out of your stomach. In that case, you might have surgery to put in a stent, a device that keeps the pathways open.
Chemotherapy. Drugs kill your cancer cells or keep them from growing. You can take them as pills or through an IV at a clinic. Chemo usually takes several weeks. The drugs can cause side effects, but your doctor can help you find ways to feel better during treatment.
Radiation. High-energy waves or particles can kill cancer cells and shrink tumors. Your doctor may use an X-ray or other machine to beam radiation at the spot where your tumor is.
Chemoradiation. Your doctor might use this mix of chemotherapy and radiation to shrink your tumor before surgery.
Targeted drugs. These newer drugs are different because they fight only cancer cells. Other treatments, like chemo and radiation, can kill healthy cells along with diseased ones. As a result, targeted therapies have fewer side effects than these other treatments.