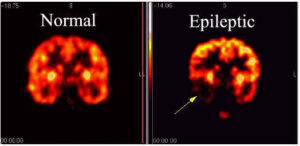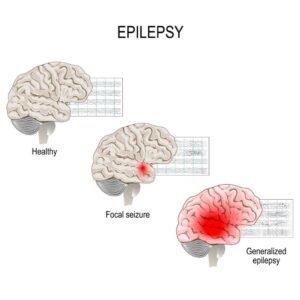
Epilepsy is a medical disorder in which seizures can occur anytime, anywhere. An epileptic seizure is an excessive, uncontrolled burst of electrical activity from nerve cells in the brain – essentially an electrical storm. There are many types of seizures that cause symptoms ranging from lightning-fast muscle jerks lasting less than a second to full body convulsions lasting two or three minutes.
Epilepsy, if not well-controlled, can greatly worsen a person’s quality of life and can cause severe injury or death. And every person with epilepsy responds in a unique and often unpredictable way to treatment, so we need as many treatments as possible.
The medical community continually tests and approves new treatments. Here are 10 treatments, both basic and advanced, that I’ve tried to rank from least to most envasive. However, almost all treatments involve some degree of risk. Discuss your options carefully with your neurologist to pick the best treatment for you as you should for any condition.
Request an appointment to discuss your epilepsy treatment options.
1. Lifestyle changes and complementary or alternative treatments
This topic is too often neglected but can have a major, positive impact on seizure control. Though there is little evidence for the effectiveness of most complementary and alternative medications, healthy lifestyle changes can go a long way toward reducing the risk of having a seizure.
Your neurologist should address these questions with you before developing a treatment plan:
● How is your sleep quality?
● Do you have chronic anxiety, depression, or excessive stress?
● Do you take other medications that may affect your epilepsy medication or directly increase the risk you will have a seizure?
● Does your use of alcohol, caffeine, or herbal remedies affect your seizure control?
The complementary and alternative therapies below can be added to your treatment plan. Because there is not a lot of medical research on their effectiveness for epilepsy, it’s important to discuss each treatment with your neurologist:
● Acupuncture
● Aerobic exercise
● Biofeedback (training to voluntarily control seizures)
● Meditation
● Yoga
I don’t hesitate to recommend aerobic exercise and meditation for all my patients — both usually are win-win treatments! It’s rare that doctors would recommend only lifestyle changes or complementary/alternative treatments for epilepsy; however, these might work sometimes.
I recently had a patient who, after experiencing a single seizure, was diagnosed with a genetic form of epilepsy. She was a student whose seizure occurred after several nights of staying up late studying and
drinking alcohol excessively. It was clear that her risk of having a seizure was higher than normal. However, it was possible that in the setting of a healthier lifestyle this might not occur. After discussing options, she and her parents decided to delay taking medication and first try to make lifestyle changes, including getting more sleep and minimizing or avoiding alcohol.
There is not much evidence that herbal remedies help with epilepsy. But medical marijuana, which is number four on this list, proves that plants have chemicals that can stop epileptic seizures (see below). At this time, we know of no other natural herb that helps with seizures. In fact, some herbs, such as the Chinese herb ma huang, can trigger or worsen seizures. Ma huang is a natural ephedra, which is similar to a stimulant hormone in our bodies. Stimulants tend to worsen seizures, so doctors are hesitant to recommend any herbal remedies at this time.
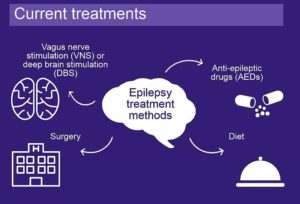
2. Diet
For many years, a special diet has been used to control certain types of epilepsy. One in particular – the ketogenic diet – gained public attention with the 1997 movie “First Do No Harm.” In this film, which is based on a true story, Meryl Streep plays the mother of a son whose epilepsy fails to respond to conventional treatments, including epilepsy surgery. She takes him to Johns Hopkins Medical Center, which pioneered the use of the ketogenic diet and demonstrated its effectiveness. Her son responded wonderfully to the diet and became seizure-free.
The ketogenic diet is strict. It severely limits carbohydrates and maximizes fats and proteins. This low-carbohydrate diet triggers ketosis, an alternate metabolic pathway in the body that somehow works against seizures. Variations in the amount of fats and proteins relative to the amount of carbohydrates are allowed. One such variation is the Modified Atkins Diet.
The ketogenic diet is challenging and is used mostly for children. A few studies have shown its effectiveness in adults, but, as one might expect, it’s difficult for most adults to maintain such a strict diet. Choosing this type of therapy requires support from experienced nurses, dietitians, and physicians who can help guide food and drink choices.
Although it may seem like the ketogenic diet has been recently created, it’s not a newly discovered way of eating. In fact, the ketogenic diet was first put into practice in the 1920s as a treatment for people with epilepsy after research demonstrated that fasting reduced seizure activity.
What exactly is the ketogenic diet? The ketogenic diet is an eating pattern that includes high amounts of fat, low to moderate amounts of protein, and very little carbohydrates. The keto diet is typically rich in foods like butter, cheese, eggs, meat, nuts, oils, seafood, and seeds. It does not allow much, if any, room for fruits, vegetables, grains, potatoes, sweets, or other carbohydrate-rich foods.
Although there are variations to the ketogenic diet, they all share a primary objective of restricting carbohydrate intake. A typical ketogenic eating plan aims for about five percent of calories from carbohydrates, 20 percent from protein, and 75 percent from dietary fats. On a 2,000-calorie-per-day ketogenic diet, this equates to about 100 calories (25 grams) of carbohydrates, 400 calories (100 grams) of protein, and 1,500 calories (167 grams) of dietary fat.
4. Medical marijuana
Medical marijuana is a term that now refers to one of more than 80 chemical compounds found in the cannabis plant – cannabidiol oil or CBD oil. This treatment came to national attention in 2013 with the story of Charlotte, a child living with Dravet syndrome in Colorado. Dravet syndrome is a severe form of genetic epilepsy, and Charlotte was having many seizures every day. CBD oil helped effectively manage Charlotte’s seizures, which has led to formal clinical studies that have proved its effectiveness.
CBD oil lacks the compound tetrahydrocannabinol (THC), so it does not appear to cause any significant mood-altering effects (“getting high”), at least compared to smoking the marijuana leaves. As of May 2018, there have been two major, scientifically rigorous clinical studies that have shown that Epidiolex, a form of CBD oil pending FDA approval, is relatively safe and effective in Dravet Syndrome and the Lennox-Gastaut Syndrome. It has been approved by the scientific advisory committee of the FDA, but final approval is pending. At this time, CBD oil is expensive. We need more research to assess its efficacy for other types of epilepsy and its possible long-term effects.
5. Medication trials
At any time, a patient may be invited to participate in a trial of an experimental medication. Since about 1993, this is how all medications have received FDA approval. Often, patients are invited to join a trial after they have failed a number of other FDA-approved medications.
The advantages of participating in a clinical trial include:
● Access to new medication
● Close support and follow-up with the epilepsy team
● The opportunity to help medical researchers develop new treatments
The goal of medication clinical trials is to make sure the drugs are safe and effective. Clinical trials are experimental studies, so there is some risk involved with participating. However, clinical research teams follow extremely strict federal, state, and hospital guidelines to ensure that the risks are minimized.
6. Extracranial neurostimulators
Neurostimulators deliver electrical stimulation to the brain. Some stimulate nerves that are not in the brain, which then transfer the electrical stimulation to the brain; we refer to these as extracranial stimulators.
The first and most common stimulation of this type is the vagus nerve stimulation (VNS), in which an electrode is wrapped around the vagus nerve on the left side of the neck and a computer battery is implanted under the skin below the collar bone. We start with the stimulator set to deliver a 30-second electrical impulse every five minutes. Each patient has a magnet that activates the device immediately and at a higher intensity if a seizure occurs. Newer versions of the VNS also can trigger a stimulus when the patient’s heartbeat goes too fast, which often happens with an epileptic seizure.
Another type of neurostimulation currently being investigated is external trigeminal nerve stimulation. This therapy stimulates a nerve on the face and does not require surgery.
7. Immunotherapy
Occasionally, epilepsy is caused by the patient’s immune system attacking the brain. Autoimmune epilepsy is a relatively recently recognized cause of epilepsy that cannot be controlled with anti-seizure medications alone.
Typically, the patient produces antibodies that attack parts of the brain, and these antibodies can be identified with a blood test. Some patients have autoimmune epilepsy, but no antibody can be identified at this time.
Treatment options include:
● High-dose steroids
● Administering a collection of human antibodies through the veins
● Plasma exchange to filter the blood of disease-causing antibodies
● Other medications that suppress the overly active immune system
8. Responsive neurostimulation (RNS®)
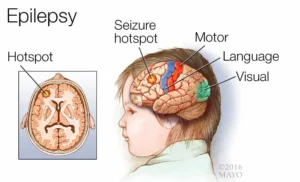
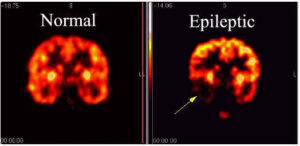
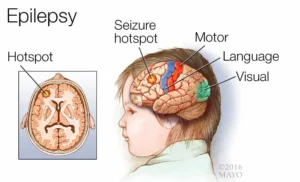
If epileptic seizures are coming from one specific region of the brain, and they cannot be stopped with medications or other therapies we have discussed, the patient can be a candidate for intracranial neurostimulation.
This first requires identifying exactly where the seizures are coming from – the seizure focus. Sometimes this can be done by recording the patient’s seizures with electrodes on the scalp using video-EEG. Often, however, we need to use intracranial electrodes to confidently determine the location of the seizure focus.
If the patient does not want surgery, if there is more than one seizure focus, or if it would be too risky to remove the seizure focus, the patient can choose intracranial automatic neurostimulation, a system developed by NeuroPace Inc.
The neurosurgeon inserts electrodes within one or more brain regions where seizures start. The electrodes detect the onset of a seizure and trigger an immediate electrical impulse in the seizure focus, which we hope will stop the seizure. It’s like fighting fire with fire. This is similar to automatic heart defibrillators for patients with potentially fatal heart arrhythmias. The main risks are scalp infections and bleeding when the electrodes are inserted.
9. Deep brain stimulation (DBS)
DBS is similar to RNS®, but the electrodes are implanted in a deep brain region called the thalamus. It has been shown effective for focal seizures, which start consistently in one specific area of the brain. Unlike RNS, it stimulates on a regular basis rather than triggering only when a seizure starts. The stimulation is directly within the brain. Also unlike RNS, it is not necessary to localize where the seizure starts. As of May 2018, the FDA has approved DBS for patients with focal epilepsy.
10. Brain surgery
Brain surgery to remove the seizure focus is the most effective method to completely stop seizures. First, we must find the seizure focus and make sure it can be safely removed. This always involves a stay in the epilepsy monitoring unit to record seizures with simultaneous video and EEG.
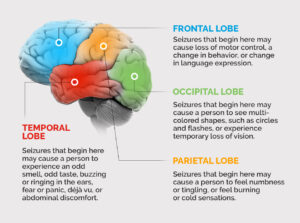
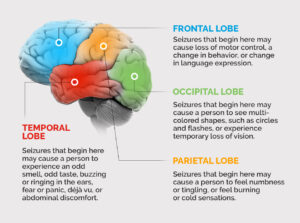
Sometimes the seizure focus cannot be determined with electrodes on the scalp, and we need to put electrodes directly within the brain. This is called intracranial EEG. The most common location in the brain for epilepsy surgery is the temporal lobe. About 60 percent to 80 percent of patients become seizure-free with this type of surgery.
A new technique is laser surgery, which involves destroying the seizure focus with heat rather than removing it. This technique is especially useful for seizures coming from deep structures in the brain and is much less invasive. Other types of surgeries include “disconnections,” in which the seizure focus is not removed but rather is prevented surgically from spreading to other areas of the brain.
The goal is to stop all seizures and to avoid any side effects that would affect the quality or safety of the patient’s life. The process sometimes can be a struggle, but we will never give up. By the time you read this, I hope there will be more treatments approved and in testing. Be sure to have a detailed discussion with your neurologist about an up-to-date treatment plan that works best for you.