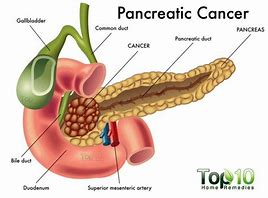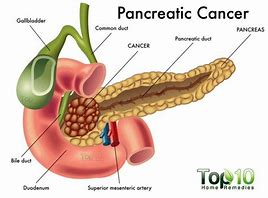
The top of pancreas attaches to the gall bile duct (allowing it into the head of the pancreas) and than there is the mesenteric artery. Blood supply to the liver, pancreas and gallbladder is via the celiac artery (or celiac axis or celiac trunk). The celiac artery also supplies the duodenum, stomach and esophagus (the foregut and its derviatives). The pancreas is also supplied to some extent by the superior mesenteric artery that goes through the head of the pancreas. This is how metastasis occurs (spreading) of pancreatic cancer can occur. These arteries allow cancerous cells thorough the head into the bile duct into the blood stream and metastasis can now happen. This can’t occur in the tail of the pancreas, its not attached to anything; which is the best place for it to occur & be diagnosed versus the head of the pancreas due to location.
Pancreatic cancer is hard to find early. The pancreas is deep inside the body, so early tumors can’t be seen or felt by health care providers during routine physical exams. People usually have no symptoms until the cancer has become very large or has already spread to other organs.
For certain types of cancer, screening tests or exams are used to look for cancer in people who have no symptoms (and who have not had that cancer before). But for pancreatic cancer, no major professional groups currently recommend routine screening in people who are at average risk. This is because no screening test has been shown to lower the risk of dying from this cancer, unfortunately.
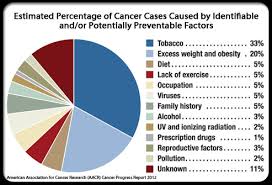
Genetic History is one of the most common risk factors in getting most cancers, including Pancreatic. Some people might be at increased risk of pancreatic cancer because of a family history of the disease (or a family history of certain other cancers). Sometimes this increased risk is due to a specific genetic syndrome.
Genetic testing looks for the gene changes that cause these inherited conditions and increase pancreatic cancer risk. The tests look for these inherited conditions, not pancreatic cancer itself. Your risk may be increased if you have one of these conditions, but it doesn’t mean that you have (or definitely will get) pancreatic cancer.
Knowing if you are at increased risk can help you and your doctor decide if you should have tests to look for pancreatic cancer early, when it might be easier to treat. But determining whether you might be at increased risk is not simple. The American Cancer Society strongly recommends that anyone thinking about genetic testing talk with a genetic counselor, nurse, or doctor (qualified to interpret and explain the test results) before getting tested. It’s important to understand what the tests can − and can’t − tell you, and what any results might mean, before deciding to be tested.
For people in families at high risk of pancreatic cancer, newer tests for detecting pancreatic cancer early may help. The two most common tests used are an endoscopic ultrasound or MRI. These tests are not used to screen the general public, but might be used for someone with a strong family history of pancreatic cancer or with a known genetic syndrome that increases their risk. Doctors have been able to find early, treatable pancreatic cancers in some members of high-risk families with these tests.
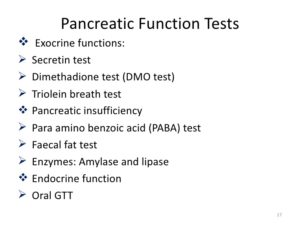
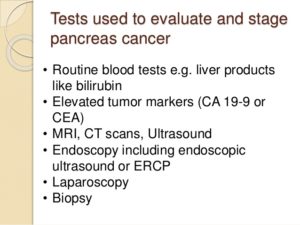
Tests for Pancreatic Cancer and even other Cancers:
A.) Doctor’s Visit
The M.D. is usually the first thing done and the M.D. will ask about your medical history to learn more about your symptoms. The doctor might also ask about possible risk factors, including smoking and your family history. Your doctor will also do a physical examine you to look for signs of pancreatic cancer or other health problems.
Doctors are also studying other new tests to try to find pancreatic cancer early. Interested families at high risk may wish to take part in studies of these new screening tests.
B.) Imaging Testing=It can be used:
- To look for suspicious areas that might be cancer
- To learn how far cancer may have spread
- To help determine if treatment is working
- To look for signs of cancer coming back after treatment
1.) CT Scan-detailed cross-sectional images of the body/pancreas. Their are special types of CT known as a multiphase CT scan or a pancreatic protocol CT scan. During this test, different sets of CT scans are taken over several minutes after you get an injection of an intravenous (IV) contrast. CT-guided needle biopsy: CT scans can also be used to guide a biopsy needle into a suspected pancreatic tumor.
2.) MRI(magnetic resonance imagery)-uses radio waves and strong magnets instead of x-rays to make detailed images of parts of your body. Most doctors prefer to look at the pancreas with CT scans, but an MRI might also be done. Special types of MRI scans that can also be used are:
-MR cholangiopancreatography (MRCP), which can be used to look at the pancreatic and bile ducts, is described below in the section on cholangiopancreatography.
-MR angiography (MRA), which looks at blood vessels, is mentioned below in the section on angiography.
3. ) Ultrasound (US) tests
These tests use sound waves to create images of organs such as the pancreas. The two most commonly used types for pancreatic cancer:
A-Abdominal ultrasound – If it’s not clear what might be causing a person’s abdominal symptoms, this might be the first test done because it is easy to do and it doesn’t expose a person to radiation. But if signs and symptoms are more likely to be caused by pancreatic cancer, a CT scan is often more useful.
B-Endoscopic ultrasound (EUS): This test is more accurate than abdominal US and can be very helpful in diagnosing pancreatic cancer. This test is done with a small US probe on the tip of an endoscope, which is a thin, flexible tube that doctors use to look inside the digestive tract and to get biopsy samples of a tumor (more invasive but more detailed in results of the pancreas).
4.) Cholangiopancreatography
Abdominal This is an imaging test that looks at the pancreatic ducts and bile ducts to see if they are blocked, narrowed, or dilated. These tests can help show if someone might have a pancreatic tumor that is blocking a duct. They can also be used to help plan surgery. If signs and symptoms are more likely to be caused by pancreatic cancer, a CT scan is often more useful.
A – Endoscopic ultrasound (EUS): This test is more accurate than abdominal US and can be very helpful in diagnosing pancreatic cancer. This test is done with a small US probe on the tip of an endoscope, which is a thin, flexible tube that doctors use to look inside the digestive tract and to get biopsy samples of a tumor.
SPYGLASS. This novel technology provides a direct view of the bile duct system, enabling our doctors to visualize lesions and narrowed areas (strictures) in the ducts and to biopsy them to see if they are cancerous. This approach ensures highly accurate sampling of the area in question. It is an excellent tool to use with confocal endomicroscopy.
B – Magnetic resonance cholangiopancreatography (MRCP):This is a non-invasive way to look at the pancreatic and bile ducts using the same type of machine used for standard MRI scans. Unlike ERCP, it does not require an infusion of a contrast dye. Because this test is non-invasive, doctors often use MRCP if the purpose is just to look at the pancreatic and bile ducts. But this test can’t be used to get biopsy samples of tumors or to place stents in ducts; like ERCP. can do also.
5.) Percutaneous transhepatic cholangiography (PTC): In this procedure, the doctor puts a thin, hollow needle through the skin of the belly and into a bile duct within the liver. A contrast dye is then injected through the needle, and x-rays are taken as it passes through the bile and pancreatic ducts. As with ERCP, this approach can also be used to take fluid or tissue samples or to place a stent into a duct to help keep it open. Because it is more invasive (and might cause more pain), PTC is not usually used unless ERCP has already been tried or can’t be done for some reason.
5.) Positron emission tomography (PET) scan
For a PET scan, you are injected with a slightly radioactive form of sugar, which collects mainly in cancer cells. A special camera is then used to create a picture of areas of radioactivity in the body.
This test is sometimes used to look for spread from exocrine pancreatic cancers.
PET/CT scan: Special machines can do both a PET and CT scan at the same time.
Pancreatoscopy. Here what is used is a small camera to visualize the pancreatic duct.
This test can help determine the stage (extent) of the cancer. It might be able to detect metastasis (spreading beyond the pancreas). See the top anatomy picture provided to understand this better by knowing the location of the organ to other parts of the body, if needed.


 In 2025
In 2025