“Common Causes of Traumatic Brain Injury:




combat injuries
Common Causes of Non-Traumatic Brain Injury:





the brain

Brain Injury Association of America (Brain Injury Awareness Month – Brain Injury Association of America)
“Common Causes of Traumatic Brain Injury:




combat injuries
Common Causes of Non-Traumatic Brain Injury:





the brain

Brain Injury Association of America (Brain Injury Awareness Month – Brain Injury Association of America)
An acquired brain injury (ABI) is an injury to the brain that is not hereditary, congenital, degenerative, or induced by birth trauma. Essentially, this type of brain injury is one that has occurred after birth. The injury results in a change to the brain’s neuronal activity, which affects the physical integrity, metabolic activity, or functional ability of nerve cells in the brain.
There are two types of acquired brain injury: traumatic and non-traumatic.
A traumatic brain injury (TBI) is defined as an alteration in brain function, or other evidence of brain pathology, caused by an external force. Traumatic impact injuries can be defined as closed (or non-penetrating) or open (penetrating).
Often referred to as an acquired brain injury, a non-traumatic brain injury causes damage to the brain by internal factors, such as a lack of oxygen, exposure to toxins, pressure from a tumor, etc.
A Brain Injury is damage to the brain that results in a loss of function such as mobility or feeling.
Traumatic Brain Injuries can result from a closed head injury or a penetrating head injury.
Penetrating Injury: A penetrating injury occurs when an object pierces the skull and enters brain tissue. As the first line of defense, the skull is particularly vulnerable to injury. Skull fractures occur when the bone of the skull cracks or breaks. A depressed skull fracture occurs when pieces of the broken skull press into the tissue of the brain. A penetrating skull fracture occurs when something pierces the skull, such as a bullet, leaving a distinct and localized injury to brain tissue. Skull fractures can cause cerebral contusion.
Brain trauma occurs when a person has an injury to the brain, and can be mild or severe. When a person sustains trauma to the brain, he or she may lose motor functions along with cognitive and physical abilities. Physicians use the Glasgow Coma Scale to determine the extent of brain trauma. This is a neurological scale that measures the level of a person’s consciousness. The Rancho Los Amigos Scale is used to monitor the recovery of the brain.
1-Traumatic brain injury occurs from external force on the head or neck. These injuries can occur from blows to the head or aggressive twisting of the neck. Some ways this could happen include falls, motor vehicle accidents, sports, and vigorous shaking. In infants, Shaken Baby Syndrome is a type of traumatic brain injury.
2-An acquired brain injury means simply you got this injury after you were born and it was caused by a condition or illness after birth. This type of injury can result from several different causes like strokes, toxic poisoning or brain tumors. Degenerative diseases and lack of oxygen may also cause this type of brain trauma. Here are some examples of acquired brain injuries:
-Bleeding in the brain which can lead to brain injury. Blood Vessels in the brain can rupture resulting in an intra-cerebral hemorrhagic (one of the causes of a stroke, its what we called Hemorrhagic Stroke). Symptoms may include headaches, loss of vision, weakness to one side of the body and eye pain to even garbled speech.
-Anoxia is another insult to the brain that can cause injury. Anoxia is a condition in which there is an absence of oxygen supply to an organ’s tissues, even if there is adequate blood flow to the tissue. Common causes of anoxia are near drowning, choking, suffocation, strangulation, heart attacks, lung damage, or very low blood pressure. They all decrease oxygen intake to the red blood cells that feed the organs nutrients (being oxygen) to our body. Anoxia is starvation to our body tissues.
Hypoxia refers to a decrease in oxygen supply rather than a complete absence of oxygen, and ischemia is inadequate blood supply, as is seen in cases in which the brain swells that causes compressing on the brain vessels near where the swelling is. In any of these cases, without adequate oxygen, a biochemical cascade called the ischemic cascade is unleashed, and the cells of the brain can die within several minutes. This type of injury is often seen in near-drowning victims, in heart attack patients, or in people who suffer significant blood loss from other injuries that decrease blood flow to the brain.
This occurs due to poisoning from chemical or biological factors that can damage the brain. Toxemia can be caused by drugs, chemicals, gases or even toxic foods.
*Meningitis is a inflammation of the lining around the brain or spinal cord, usually due to infection; Neck stiffness, headache, fever, and confusion are common symptoms.
*Encephalitis (en-sef-uh-LIE-tis) is inflammation of the brain. Viral infections are the most common cause of the condition. Encephalitis can cause flu-like symptoms, such as a fever or severe headache. It can also cause confused thinking, seizures, or problems with senses or movement.
*HIV can lead to brain injury. HIV, can affect the brain in different ways. HIV-meningoencephalitis is infection of the brain and the lining of the brain by the HIV virus. It occurs shortly after the person is first infected with HIV and may cause headache, neck stiffness, drowsiness, confusion and/or seizures. HIV-encephalopathy (HIV-associated dementia) is the result of damage to the brain by longstanding HIV infection. It is a form of dementia and occurs in advanced HIV infection. Mild Neurocognitive Disorder is problems with thinking and memory in HIV, however is not as severe as HIV-encephalopathy. Unlike HIV-encephalopathy it can occur early in HIV infection and is not a feature of Aquired Immune Deficiency Syndrome – AIDS.
*Lastly, Herpes. There are two types of herpes simplex virus (HSV). Either type can cause encephalitis. HSV type 1 (HSV-1) is usually responsible for cold sores or fever blisters around your mouth, and HSV type 2 (HSV-2) commonly causes genital herpes. Encephalitis caused by HSV-1 is rare, but it has the potential to cause significant brain damage or death.
*Other herpes viruses. Other herpes viruses that may cause encephalitis include the Epstein-Barr virus, which commonly causes infectious mononucleosis, and the varicella-zoster virus, which commonly causes chickenpox and shingles.*Viral infections due to blood sucking insects like mosquitoes and ticks to animals with rabies a rapid progression to encephalitis once symptoms begin. Rabies is a rare cause of encephalitis in the U.S.
Rehabilitation programs may vary depending on the type of brain injury and estimated recovery time. Treatment usually consists of physical therapy and daily activities. In extreme cases, patients may need to learn how to read and write again.
Therapy for brain trauma typically takes place on an outpatient basis or through an assisted living facility. Therapy may last several weeks, months or even years, and sometimes the patient is not able to make a full recovery.
It may not always be obvious when a person has sustained a brain injury. The patient may have hit his or her head and not have symptoms until a few hours later. Some signs of a possible brain injury are headaches, confusion and loss of memory. If brain trauma is not treated, it could cause permanent damage or death.
Brain injuries can affect the patient and the patient’s family, with emotional and financial hardship. When problems arise with treatment or financial issues, a brain injury lawyer or specialist may need to intervene.
REVISED 2/25/2021 By Elizabeth Lynch RN BSN Cardiac/Stroke Certified (RN 34.5 Years)
“Based on the most recent data available, in the United States in 2021, 141,902 new colorectal cancers were reported and in 2022, 52,967 people died from colorectal cancer.
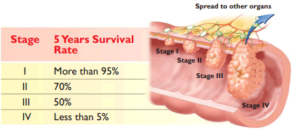
From 2017 to 2021, about 1 in 3 colorectal cancer cases were diagnosed at a localized stage, meaning the cancer had not spread outside the colon or rectum. Almost 4 in 10 colorectal cancers were found at a regional stage (the cancer had spread to nearby lymph nodes, tissues, or organs), and about 2 in 10 were found at a distant stage (the cancer had spread to distant parts of the body).
Overall, 64% of colorectal cancer patients had not died from their cancer 5 years later. However, survival varied by stage at diagnosis.
Survival is higher when colorectal cancer is found before it spreads to other parts of the body. Screening tests can prevent colorectal cancer or find it early, when treatment works best.”
Center for Disease Control and Prevention – CDC (U.S. Cancer Statistics Colorectal Cancer Stat Bite | U.S. Cancer Statistics | CDC)
A colectomy (or colon resection) is abdominal surgery that removes the section of colon where the tumor is located, tissue containing blood and lymph vessels surrounding the colon (mesentery), healthy tissue margins on either side and, if possible, at least 12 lymph nodes. Then the remaining ends of colon are reconnected with sutures or staples. This connection is called an anastomosis.
There are two types of surgery:
Treatment of node-negative stage II colon cancer is controversial. While surgery to remove the tumor in the colon is universally accepted as initial treatment, the value of chemotherapy after that surgery to keep cancer from recurring (coming back) is hard for patients and doctors to judge.
It’s estimated that between four and five percent of patients with stage II colon cancer will benefit from chemotherapy. However, there are also side effects, some severe, associated with chemotherapy. Very few patients will die as a result of chemotherapy.
Because of the risks of treatment, researchers are looking for ways to identify patients who are at higher risk for recurrence, who are most likely to benefit from chemotherapy.
Some factors have been identified that lead to higher risk for stage II patients including:
Stage III colorectal cancers have spread outside the colon to one or more lymph nodes (small structures that are found throughout the body that produce and store cells that fight infection). Tumors within the colon wall, which also involve the lymph nodes are classified as stage IIIA, while tumors that have grown through the colon wall and have spread to one to four lymph nodes are classified as stage IIIB cancers. Those tumors, which have spread to more than four lymph nodes are classified as stage IIIC colon cancers.
Treatment involves:
The five-year survival rate for stage III colon cancer is about 64%. Patients with one to four positive lymph nodes have a higher survival rate than people with more than five positive lymph nodes.
Stage IV Colorectal cancer treatments:
Stage IV colorectal cancers have spread outside the colon to other parts of the body, such as the liver or the lungs. Cancer that has spread is also called “metastatic.” The tumor can be any size and may or may not include affected lymph nodes (small structures that are found throughout the body that produce and store cells that fight infection).
Treatment may include:
The five-year survival rate for stage IV colon cancer is nearly 8% or less.
“After someone is diagnosed with colorectal cancer, doctors will try to figure out if it has spread, and if so, how far. This process is called staging. The stage of a cancer describes how much cancer is in the body. It helps determine how serious the cancer is and how best to treat it. Doctors also use a cancer’s stage when talking about survival statistics.
The earliest stage of colorectal cancers is called stage 0 (a very early cancer), and then range from stages I (1) through IV (4). As a rule, the lower the number, the less the cancer has spread.
The staging system most often used for colorectal cancer is the American Joint Committee on Cancer (AJCC) TNM system, which is based on 3 key pieces of information:
American Cancer Society (Colorectal Cancer Stages | Rectal Cancer Staging | Colon Cancer Staging | American Cancer Society)
Part II Treatment & Care
Many colon cancer treatment options are available for colorectal cancer, including surgery, chemotherapy, and radiation. Here’s what to expect from each type of treatment and tips for recovery.
Polyp Removal and Other Precancerous Conditions
Precancerous conditions of the colon or rectum are changes to cells that make them more likely to develop into cancer. These conditions are not yet cancer, but there is a higher chance these abnormal changes will become colorectal cancer.
–adenomas
–hereditary colorectal syndromes
If you have a precancerous condition, you will likely have regular follow-up and screening tests to find cancer as early as possible if it develops. Some precancerous conditions can be treated with surgery to help reduce the risk that they will become cancer.
Stages of the cancer with TNM system for colorectal cancer helps determine the RX.
The most commonly used colorectal cancer staging system is known as the TNM system, which has been established by the American Joint Committee on Cancer. The TNM staging system looks at three key factors to determine the stage of cancer:
A number (0-4 stages) or the letter X is assigned to each factor. Using this colorectal cancer staging system, a higher number indicates increasing severity. For instance, a T1 score indicates a smaller tumor than a T2 score. The letter X means the information could not be assessed.
Stages of colorectal cancer diagnosis occurs in conjunction with the following TNM categories:
Once the T, N and M scores have been assigned, an overall stage is determined, and thus treatment options can be explored.
Here’s a quick rundown of the options available for colorectal cancer treatment from surgery to cutting-edge biologic therapy.
Colorectal Cancer: Treatment by Stages
Chemotherapy is not recommended for stage 0 colon cancer.
Colectomy (resection): Abdominal surgery to remove the section of colon where the tumor is located, tissue containing blood and lymph vessels surrounding the colon (mesentery), healthy tissue margins on either side, and at least 12 lymph nodes, if possible. Then the remaining ends of colon are reconnected with sutures or staples. This connection is called an anastomosis.
Open colectomy: An incision is made in the abdomen, surgery performed through the opening, and the incision closed with sutures and/or staples.
Laparoscopic colectomy: Three small keyhole incisions are made to insert a lighted instrument and specially designed surgical instruments that can be manipulated within the abdomen. Sometimes an incision is made just long enough for the surgeon’s hand to assist during laparoscopy.
Chemotherapy is not recommended for stage I colon cancer.
Part III on continuation of treatments of other stages of this condition (Stage II & III)
“Colon cancer is a growth of cells that begins in a part of the large intestine called the colon. The colon is the first and longest part of the large intestine. The large intestine is the last part of the digestive system. The digestive system breaks down food for the body to use.
Colon cancer typically affects older adults, though it can happen at any age. It usually begins as small clumps of cells called polyps that form inside the colon. Polyps generally aren’t cancerous, but some can turn into colon cancers over time.
Polyps often don’t cause symptoms. For this reason, doctors recommend regular screening tests to look for polyps in the colon. Finding and removing polyps helps prevent colon cancer.”
MAYO CLINIC (Colon cancer – Symptoms and causes – Mayo Clinic)
Colorectal cancer is cancer that develops in the tissues of the colon and/or rectum. The colon and the rectum are both found in the lower part of the gastrointestinal (digestive) system. They form a long, muscular tube called the large intestine (or large bowel). The colon absorbs food and water and stores waste. The rectum is responsible for passing waste from the body.
If the cancer began in the colon, which is the first four to five feet of the large intestine, it may be referred to as colon cancer. If the cancer began in the rectum, which is the last several inches of the large intestine leading to the anus, it is called rectal cancer.
Colorectal cancer starts in the inner lining of the colon and/or rectum, slowly growing through some or all of its layers. It typically starts as a growth of tissue called a polyp. A particular type of polyp, called an adenoma, can then develop into cancer.
Adenocarcinoma is the most common type of colorectal cancer. Other colorectal cancers include gastrointestinal carcinoid tumors, gastrointestinal stromal tumors, primary colorectal lymphoma, leiomyosarcoma, melanoma and squamous cell carcinoma.
Cancer is a disease in which cells in the body grow out of control. When cancer starts in the colon or rectum, it is called colorectal cancer. Sometimes it is called colon cancer, for short.
Colorectal cancer affects men and women of all racial and ethnic groups, and is most often found in people aged 50 years or older. In the United States, it is the third most common cancer for men and women.
Of cancers that affect both men and women, colorectal cancer is the second leading cancer killer in the United States, but it doesn’t have to be.
Colorectal cancer screening saves lives.
Screening can find precancerous polyps—abnormal growths in the colon or rectum—so that they can be removed before turning into cancer. Screening also helps find colorectal cancer at an early stage, when treatment often leads to a cure. About nine out of every 10 people whose colorectal cancers are found early and treated appropriately are still alive five years later.
If you are aged 50 or older, get screened now. If you think you may be at higher than average risk for colorectal cancer, speak with your doctor about getting screened early.
While screening rates have increased in the U.S., not enough people are getting screened for colorectal cancer. In 2012, 65% of U.S. adults were up-to-date with colorectal cancer screening; 7% had been screened, but were not up-to-date; and 28% had never been screened.
Your risk of getting colorectal cancer increases as you get older. More than 90% of cases occur in people who are 50 years old or older.
Other risk factors include having:
*Inflammatory bowel disease, Crohn’s disease, or ulcerative colitis.
*A personal or family history of colorectal cancer or colorectal polyps.
*A genetic syndrome such as familial adenomatous polyposis (FAP)hereditary non-polyposis colorectal cancer (Lynch syndrome).
Lifestyle factors that may contribute to an increased risk of colorectal cancer include—
*Treatment= Get details on treatment on Part II tomorrow’s article Thurs.
Colon Polyp Removal and Other Precancerous Conditions
Learn how colon polyps are removed and why it’s so important to stay on top of these and other precancerous conditions.
Here’s a quick rundown of the options available for colorectal cancer treatment from surgery to cutting-edge biologic therapy.
Colon Cancer: Treatment by Stage
Here you’ll find detailed information on how the various stages of colon cancer are treated — from stage 0 to stage IV and also recurrent colon cancer.
Rectal Cancer Treatment by Stage
Here you’ll find detailed information on how the various stages of rectal cancer are treated — from stage 0 to stage IV and also recurrent rectal cancer.
Learn about the different ways chemotherapy is used to treat colon cancer and rectal cancer and the side effects of commonly used chemotherapy drugs.
Centers for Disease Prevention – CDC (Heart Disease Facts | Heart Disease | CDC)
This year marks the 50th Anniversary of American Heart Month. For the past 55 years, the American Heart Association (AHA) has used the month of February to partner with the media, medical providers and community organizations to spread the word about heart disease prevention and treatment. Heart disease is a leading cause of death for both men and women. Over the years, the American Heart Association has sponsored awareness and education campaigns as well as medical research funding, investing more than $3.5 billion into studies. According to the AMA, this is the most amount of funding of any entity outside the federal government.
The AHA provides the following reminders to encourage you to live a heart-healthy lifestyle: