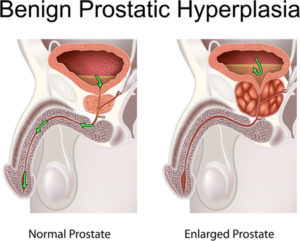
Normal Prostate vs. Benign Prostatic Hyperplasia
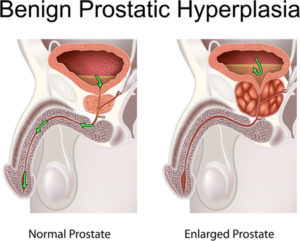
The prostate is a walnut-shaped gland that is part of the male reproductive system. The main function of the prostate is to make a fluid that goes into semen. Prostate fluid is essential for a man’s fertility. The gland surrounds the urethra at the neck of the bladder. The bladder neck is the area where the urethra joins the bladder. The bladder and urethra are parts of the lower urinary tract. The prostate has two or more lobes, or sections, enclosed by an outer layer of tissue, and it is in front of the rectum, just below the bladder. The urethra is the tube that carries urine from the bladder to the outside of the body. In men, the urethra also carries semen out through the penis.
What is benign prostatic hyperplasia?
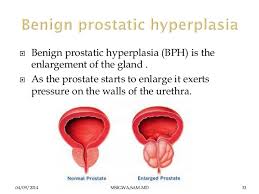
Benign prostatic hyperplasia––also called BPH––is a condition in men in which the prostate gland is enlarged and not cancerous. Benign prostatic hyperplasia is also called benign prostatic hypertrophy or benign prostatic obstruction.
The prostate goes through two main growth periods as a man ages. The first occurs early in puberty, when the prostate doubles in size. The second phase of growth begins around age 25 and continues during most of a man’s life. Benign prostatic hyperplasia often occurs with the second growth phase.
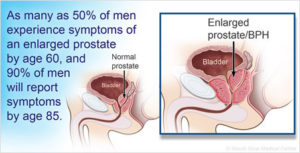
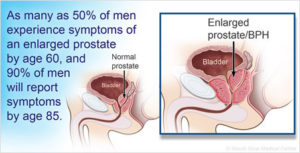
As the prostate enlarges, the gland presses against and pinches the urethra. The bladder wall becomes thicker. Eventually, the bladder may weaken and lose the ability to empty completely, leaving some urine in the bladder. The narrowing of the urethra and urinary retention––the inability to empty the bladder completely––cause many of the problems associated with benign prostatic hyperplasia.
Ending line the prostate enlarges pushes up to the superior both front and back aspects of the penis (just below the urinary bladder) narrowing the urethra in the penis shaft (on both sides of the urethra) causing urination difficulty and frequently urinating. (See figure below the picture shows in the top part the urinary bladder and the prostate below it Left normal Right BPH).
What causes benign prostatic hyperplasia?
The cause of benign prostatic hyperplasia is not well understood; however, it occurs mainly in older men. Benign prostatic hyperplasia does not develop in men whose testicles were removed before puberty. For this reason, some researchers believe factors related to aging and the testicles may cause benign prostatic hyperplasia.
Throughout their lives, men produce testosterone, a male hormone, and small amounts of estrogen, a female hormone. As men age, the amount of active testosterone in their blood decreases, which leaves a higher proportion of estrogen. Scientific studies have suggested that benign prostatic hyperplasia may occur because the higher proportion of estrogen within the prostate increases the activity of substances that promote prostate cell growth.
Another theory focuses on dihydrotestosterone (DHT), a male hormone that plays a role in prostate development and growth. Some research has indicated that even with a drop in blood testosterone levels, older men continue to produce and accumulate high levels of DHT in the prostate. This accumulation of DHT may encourage prostate cells to continue to grow. Scientists have noted that men who do not produce DHT do not develop benign prostatic hyperplasia.
How common is BPH?
Benign prostatic hyperplasia is the most common prostate problem for men older than age 50. In 2010, as many as 14 million men in the United States had lower urinary tract symptoms suggestive of benign prostatic hyperplasia. Although benign prostatic hyperplasia rarely causes symptoms before age 40, the occurrence and symptoms increase with age. Benign prostatic hyperplasia affects about 50 percent of men between the ages of 51 and 60 and up to 90 percent of men older than 80.
Signs and Symptoms
BPH, the prostate gland grows in size. It may compress the urethra which courses through the center of the prostate. This can impede the flow of urine from the bladder through the urethra to the outside. It can cause urine to back up in the bladder (retention) leading to the need to urinate frequently during the day and night. Other common symptoms include a slow flow of urine, the need to urinate urgently and difficulty starting the urinary stream. More serious problems include urinary tract infections=pain in pelvic region and complete blockage of the urethra, which would be a medical emergency and can lead injury to the kidneys.
Treatment:
Is BPH always treated?
No. Treatment of BPH is usually reserved for men with significant symptoms. Watchful waiting with medical monitoring once a year is appropriate for most men with BPH.
How is BPH treated?
There are several different ways to treat BPH:
Men should carefully weigh the risks and benefits of each of these options. Prostate surgery has traditionally been seen as offering the most benefits for BPH but unfortunately carries the most risks.
- Watchful waiting is often chosen by men who are not bothered by symptoms of BPH. They have no treatment but get regular checkups and wait to see whether or not the condition gets worse.
Medical Treatment through drugs is used by some men rangaing from alpha blockers relax the smooth muscles of the prostate, and the bladder neck. An example of these meds are tamzulosin (Flomax), alfusozin, (Uroxatral), and older medications such as terazosin (Hytrin), slidosin (Rapaflo) or doxazosin (Cardura).
Also 5-alpha reductase inhibitors block the conversion of the male hormone testosterone into its active form in the prostate. Examples of 5-alpha reductase inhibitors include Finasteride (Proscar) and dutasteride (Avodart). Side effects of finasteride may include declining interest in sex, problems getting an erection, and problems with ejaculation.
Surgery or office procedures may also be used to treat BPH, most commonly in men who have not responded satisfactorily to medication or those who have more severe problems, such as a complete inability to urinate.
- Transurethral resection of the prostate (TURP) has been used for the longest period of time. After the patient is given anesthesia, the doctor inserts a special instrument into the urethra through the penis. With the instrument, the doctor then shaves away part of the inner prostate to relieve the outflow of urine from the bladder.
- Laser procedures: A number of laser procedures are available, some of which can be performed in the doctor’s office with minimal anesthesia. These procedures also involve the removal of obstructing prostate tissue. They are generally associated with less bleeding and quicker recovery than TURP.
- Microwave therapy: This procedure is generally performed in the office and involves the use of microwave energy delivered to the prostate to kill some of the cells leading eventually to shrinkage of the prostate.