Do your research before definitely deciding on a surgeon and hospital doing this treatment. It’s your body, not theirs. See what their history is and why they are so great to select in doing this invasive procedure. We have many in N.Y. just do your research. The higher the odds less problems with more experience and good hospital overall reviews.
Hospital of Special Surgery (HSS) is nationally ranked No. 1 in orthopedics (for the ninth consecutive year) and No. 3 in rheumatology by U.S.News & World Report (2018-2019). HSS has been among the top-ranked hospitals for orthopedics and rheumatology for 27 consecutive years. Hospital of Special Surgery is in Manhattan, N.Y.
Because an infection can be a devastating outcome for an orthopedic patient, Hospital for Special Surgery takes infection control extremely seriously and is proud of the recognition received for our significantly low infection rates.
Recommended as an excellent hospital in NY understanding hip surgical procedures is Hospital of Special Surgery in Manhattan and also a doctor on board their understanding hip surgery is Dr. Padgett.
From 1985-1989, Dr. Padgett was a resident in orthopedic surgery at Hospital for Special Surgery and subsequently performed a one-year postdoctoral fellowship at The Rush Presbyterian Medical Center in Chicago in Adult Reconstructive Surgery of the hip and knee (1989-90). From 1990-1993, Dr. Padgett was the Director of the Adult Reconstructive Service at the Naval Hospital, San Diego and developed the Adult Reconstructive Education Program. In 1991, Dr. Padgett was deployed to the Persian Gulf with Fleet Hospital #6 in support of military operation during Operations Desert Shield and Desert Storm.
In 1993, Dr. Padgett joined Hospital for Special Surgery as an attending surgeon on the Hip and Knee Service. In 2006, Dr. Padgett became the chief of the Hip Service, and in 2008 chief of the Adult Reconstruction and Joint Replacement Service. In addition to his duties at Hospital for Special Surgery, Dr. Padgett is also a consulting physician for the Bronx V.A. Medical Center.
Know your M.D. and Hospital’s reputation on doing this particular surgery:
Under the U.S. News for Health they do ranking of hospitals in the U.S.
Hospital for Special Surgery in New York, N.Y. is nationally ranked in 2 adult specialties and 1 pediatric specialty and rated high performing in 2 adult procedures and conditions. It is an orthopedic facility. It scored high in patient safety, demonstrating commitment to reducing accidents and medical mistakes. It is a teaching hospital.
Rankings & Ratings
The U.S. News analysis of hospitals includes data from nearly 5,000 centers across multiple medical specialties, procedures and medical conditions including neurology, orthopedics, psychiatry and more. Scores are based on a variety of patient outcome and care-related factors, such as patient safety and nurse staffing. U.S. News ranks hospitals in 16 adult and 10 pediatric specialties. Hospitals also receive a rating in 9 common procedures and conditions, including hip replacement and COPD. Read more about how we rank and rate hospitals.
Specialties at this Hospital of Special Surgery in NYC
Children’s Specialties at this Hospital (Special Surgery in NYC)
Procedures and Conditions at this Hospital of Special Surgery in NYC.
Do your research.
What should you consider when choosing this hip surgery?
It’s the time you are expecting to get this done and are you an appropriate candidate.
Timing of surgery is another important consideration in predicting successful outcomes. “Generally I advise patients that it’s reasonable to consider surgery when the disability and pain in the knee or hip is affecting your quality of life and you’ve tried all other means available to alleviate your symptoms,” stated Dr. Russell Windsor.
If learning from this topic, you might be asking yourself who is Dr. Russell Windsor? Go no further here is who he is:
Dr. Russell E. Windsor received his medical education at the Georgetown, Thomas Jefferson, and Cornell Universities. He completed his orthopedic training at the University of Pennsylvania and did a Fellowship in Knee Reconstructive Surgery at the Hospital for Special Surgery under John Insall, MD, who was one of the original developers and father of total knee replacement surgery. Dr. Windsor has presented his work and served as faculty member in over 250 national and international seminars and has written over 60 original publications and contributed chapters in reconstructive surgery in 40 textbooks. He has been featured on Good Morning America with Diane Sawyer and the NBC Today Show where he discussed total knee replacement and total hip replacement surgery.
Dr. Windsor was Chief of the Knee Service at the Hospital for Special Surgery between 1990 and 2006 and was President of the American Knee Society in 2005. He has been an active design consultant for various total knee replacement designs and has approximately 15 American and international patents for the design of Zimmer’s unicompartmental replacements (ZUK) and rotating hinge knee replacement (RHK).
His research concentrates on minimally invasive unicompartmental and total knee replacement. Additionally, he has a special interest in total knee replacement in the athlete and the younger, active patient with arthritis. He has a substantial experience in revision surgery and has performed thousands of knee and hip replacements. He also is a world expert in gender specific knee replacement and ligament reconstruction. His expertise is also strong in sports medicine of the knee. Again, do your research.
Prospective patients should also take into account the importance of having surgery while they are otherwise in good health. In the past, some middle-aged patients have elected to wait for a joint replacement, because of their concern about the longevity of the new joint; that is, that a second joint replacement surgery might eventually be required. However, not only does the data indicate that knee and hip replacements are lasting as long as twenty-five or even thirty years, but delaying surgery may result in the surrounding muscles becoming de-conditioned owing to reduced function. In turn, this may make recovery from surgery more difficult.
Older individuals, including those in their 80s and 90s may also want to consider the benefits of scheduling surgery sooner versus “living with” disability. While the ability to tolerate surgery and recovery, as well as the existence of coexisting medical conditions must be taken into account, recent data shows that joint replacement that helps to preserve function can have an overall positive effect on the health of older patients. Those who are able to be more active have a reduced risk – when compared to their more sedentary counterparts – of various medical conditions including pulmonary embolism, deep vein thrombosis and pneumonia.
“Knee and hip replacement surgery improves the quality of life of thousands of patients each year,” Dr. Windsor notes. “However, both advertising claims and misinformation on the Internet can lead to confusion about which implant works best or even an exaggerated sense of risk associated with the surgery. In many cases, a discussion with your surgeon can clarify implant options and establish realistic expectations about hip and knee replacement surgery.”
“As with any surgery there is always some risk involved. There have been a few knee and hip implant systems that have not worked well,” Dr. Windsor says, “and isolated recalls of specific models have occurred. But people should be aware of the shared commitment on the part of industry, hospitals, and surgeons to the welfare of the patient and to addressing any problems with implants that do occur.”
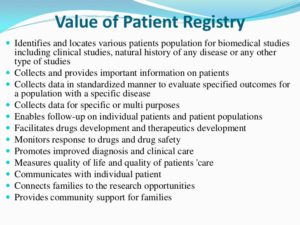
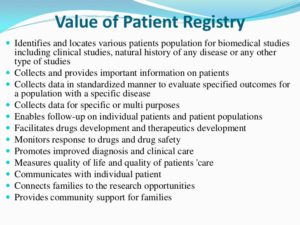
One method to monitor performance of hip and knee implants is through a patient registry. The orthopedic surgeons at HSS are dedicated to following the long-term patient centered outcomes of joint replacement surgery in our Total Joint Prospective Clinical Outcomes Research Registry. Using this registry, long term implant performance may be followed and hopefully surgeons can identify as early as possible any poor performing implants.