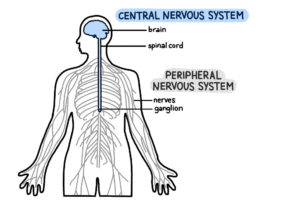
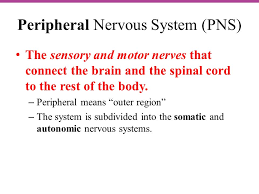
Peripheral neuropathy is a type of damage to the nervous system. Specifically, it is a problem with your peripheral nervous system. This is the network of nerves that sends information from your brain and spinal cord (central nervous system) to the rest of your body.
There are more than 100 types of peripheral neuropathy, each with its own set of symptoms and prognosis. Peripheral neuropathy has many different causes.
Most common causes of peripheral neuropathy in the U.S. is diabetes.
Symptoms can range from tingling or numbness in a certain body part to more serious effects, such as burning pain or paralysis.
Peripheral neuropathy has many different causes. Some people inherit the disorder from their parents. Others develop it because of an injury or another disorder.
In many cases, a different type of problem, such as a kidney condition or a hormone imbalance, leads to peripheral neuropathy. One of the most common causes of peripheral neuropathy in the U.S. is diabetes.
CAUSES OF PERIPHERAL NEUROPATHY:
#1 DIABETES
Trauma: Injuries from falls, car accidents, fractures or sports activities can result in neuropathy. Compression of the nerves due to repetitive stress or narrowing of the space through which nerves run are other causes.
Autoimmune disorders and infections: Guillain-Barré syndrome, lupus, rheumatoid arthritis, Sjogren’s syndrome and chronic inflammatory demyelinating polyneuropathy are autoimmune disorders that can cause neuropathy. Infections including chickenpox, shingles, human immunodeficiency virus (HIV), herpes, syphilis, Lyme disease, leprosy, West Nile virus, Epstein-Barr virus and hepatitis C can also cause neuropathy.
Other health conditions: Neuropathy can result from kidney disorders, liver disorders, hypothyroidism, tumors (cancer-causing or benign) that press on nerves or invade their space, myeloma, lymphoma and monoclonal gammopathy.
Medications and poisons: Some antibiotics, some anti-seizures medications and some HIV medications among others can cause neuropathy. Some treatments, including cancer chemotherapy and radiation, can damage peripheral nerves. Exposure to toxic substances such as heavy metals (including lead and mercury) and industrial chemicals, especially solvents, can also affect nerve function.
Vascular disorders: Neuropathy can occur when blood flow to the arms and legs is decreased or slowed by inflammation, blood clots, or other blood vessel disorders. Decreased blood flow deprives the nerve cells of oxygen, causing nerve damage or nerve cell death. Vascular problems can be caused by vasculitis, smoking and diabetes.
Abnormal vitamin levels and alcoholism: Proper levels of vitamins E, B1, B6, B12, and niacin are important for healthy nerve function. Chronic alcoholism, which typically results in lack of a well-rounded diet, robs the body of thiamine and other essential nutrients needed for nerve function. Alcohol may also be directly toxic to peripheral nerves.
Inherited disorders: Charcot-Marie-Tooth (CMT) disease is the most common hereditary neuropathy. CMT causes weakness in the foot and lower leg muscles and can also affect the muscles in the hands. Familial amyloidosis, Fabry disease and metachromatic leukodystrophy are other examples of inherited disorders that can cause neuropathy.
No known cause: Some cases of neuropathy have no known cause.
There are types of Peripheral Neuropathy:
There are more than 100 types of peripheral neuropathy, each with its own set of symptoms and prognosis. To help doctors classify them, they are often broken down into the following categories:
- Motor neuropathy. This is damage to the nerves that control muscles and movement in the body, such as moving your hands and arms or talking.
- Sensory neuropathy. Sensory nerves control what you feel, such as pain, temperature or a light touch. Sensory neuropathy affects these groups of nerves.
- Autonomic nerve neuropathy. Autonomic nerves control functions that you are not conscious of, such as breathing and heartbeat. Damage to these nerves can be serious.
- Combination neuropathies. You may have a mix of 2 or 3 of these other types of neuropathies, such as a sensory-motor neuropathy.
Signs and Symptoms remember vary from patient to patient:
The symptoms of peripheral neuropathy vary based on the type that you have and what part of the body is affected. Symptoms can range from tingling or numbness in a certain body part to more serious effects such as burning pain or paralysis.
- Muscle weakness, Cramps, Muscle twitching to Loss of muscle and bone
- Changes in skin, hair, or nails
- Numbness, Loss of sensation or feeling in body parts
- Loss of balance or other functions as a side effect of the loss of feeling in the legs, arms, or other body parts
- Loss of pain or sensation that can put you at risk, such as not feeling an impending heart attack or limb pain
- Emotional disturbances, Sleep disruptions
- Inability to sweat properly, leading to heat intolerance
- Loss of bladder control, leading to infection or incontinence
- Dizziness, lightheadedness, or fainting because of a loss of control over blood pressure
- Diarrhea, constipation, or incontinence related to nerve damage in the intestines or digestive tract
- Trouble eating or swallowing
- Life-threatening symptoms, such as difficulty breathing or irregular heartbeat
The symptoms of peripheral neuropathy may look like other conditions or medical problems. Always see your healthcare provider for a diagnosis.
The most common type of peripheral neuropathy is diabetic neuropathy, caused by a high sugar level and resulting in nerve fiber damage in your legs and feet.