President Ronald Reagan

“Lewy bodies are clumps of abnormal protein particles that, for reasons that are not fully understood, accumulate in the brain. These deposits cause a form of dementia called Lewy body dementia, or LBD — which is what the late actor and comedian Robin Williams suffered from.
LBD is not the same as Parkinson’s, but the two are closely related: LBD causes some or all of the motor symptoms of Parkinson’s. More than 1 million people in the U.S. are affected by Lewy body dementia, according to the Lewy Body Dementia Association.”
John Hopkins Medicine
1-Most important is getting an experienced clinician within the medical community who should perform a diagnostic evaluation. If one is not available, the neurology department of the nearest medical university should be able to recommend appropriate resources or may even provide an experienced diagnostic team skilled in Lewy body dementia.
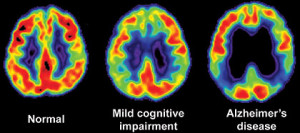
A thorough dementia diagnostic evaluation includes physical and neurological examinations, patient and family interviews (including a detailed lifestyle and medical history), and neuro-psychological and mental status tests. The patient’s functional ability, attention, language, visuospatial skills, memory and executive functioning are assessed.
Than further diagnostic tooling to help diagnose LBD:
2- A brain imaging (CT or MRI scans)
3-Blood tests
4-Other laboratory studies may be performed.
The evaluation will provide a clinical diagnosis. Unfortunately, currently, a conclusive diagnosis of LBD can be obtained only from a postmortem autopsy for which arrangements should be made in advance. Some research studies may offer brain autopsies as part of their protocols. Participating in research studies is a good way to benefit others with Lewy Body Dementia. Though it is hard to do this if you only get diagnosed with this after you die being misdiagnosed previously when alive, like Robin Williams through a autopsy. So the point is when symptoms resembling dementia or better Lewy Body Dementia go to an expert doctor in this
Medications are one of the most controversial subjects in dealing with LBD. A medication that doesn’t work for one person may work for another person. Become knowledgeable about LBD treatments and medication sensitivities.
Prescribing should only be done by a physician who is thoroughly knowledgeable about LBD. With new medications and even ‘over-the-counter,’ the patient should be closely monitored. At the first sign of an adverse reaction, consult with the patient’s physician. Consider joining the online caregiver support groups to see what others have observed with prescription and over-the-counter medicines.
Advanced age is considered to be the greatest risk factor for Lewy Body Dementia, with onset typically, but not always, between the ages of 50 and 85. Some cases have been reported much earlier. It appears to affect slightly more men than women. Having a family member with Lewy Body Dementia may increase a person’s risk. Observational studies suggest that adopting a healthy lifestyle (exercise, mental stimulation, nutrition) might delay age-associated dementias.
The recruitment of LBD patients for participation in clinical trials for studies on LBD, other dementias and Parkinsonian studies is now steadily increasing.
Defining the stages of disease progression for LBD is difficult. The symptoms, medicine management and duration of LBD vary greatly from person to person. To further complicate the stages assessment, LBD has a progressive but vacillating clinical course, and one of its defining symptoms is fluctuating levels of cognitive abilities, alertness and attention. Sudden decline is often caused by medications, infections or other compromises to the immune system and usually the person with LBD returns to their baseline upon resolution of the problem. But for some individuals, it may also be due to the natural course of the disease.
Come back tomorrow to learn treatments for LBD!
“Lewy body dementia, also known as dementia with Lewy bodies, is the second most common type of progressive dementia after Alzheimer’s disease. Protein deposits, called Lewy bodies, develop in nerve cells in the brain regions involved in thinking, memory and movement (motor control). Lewy body dementia causes a progressive decline in mental abilities. People with Lewy body dementia might have visual hallucinations and changes in alertness and attention.”
MAYO CLINIC
Learn the S/S Robin Williams had,which where 3 of 4 of these:
“Who was Lewy? In the early 1900s, while researching Parkinson’s disease, the scientist Friederich H. Lewy discovered abnormal protein deposits that disrupt the brain’s normal functioning. These Lewy body proteins are found in an area of the brain stem where they deplete the neurotransmitter dopamine, causing Parkinsonian symptoms.
In Lewy Body Dementia [LBD], these abnormal proteins are diffuse throughout other areas of the brain, including the cerebral cortex. The brain chemical acetylcholine is depleted, causing disruption of perception, thinking and behavior. Lewy body disease exists either in pure form, or in conjunction with other brain changes, including those typically seen in Alzheimer’s disease and Parkinson’s disease.”
We all know Robin Williams and initially he was presented in the news as committing suicide but in the past few years it has been presented by doctors that he died of LBD which makes more sense, for a man who had it all to many with Parkinson’s Disease. Robin all his life wanted to make others smile and laugh, never did he come across as a depressed unhappy man. We all have our ups and downs along our journey living, which is a part of life. Killing yourself is a severe extreme and you know the news (jump at the first juicy article to make it big or and if we are wrong will admit it or possibly apologize later, sad). The disease killed him in making him think to do suicide.
LBD is not a rare disease. It affects an estimated 1.4 million individuals and their families in the United States. Because LBD symptoms can closely resemble other more commonly known diseases like Alzheimer’s and Parkinson’s, it is currently widely underdiagnosed. Many doctors or other medical professionals still are not familiar with LBD.
Lewy body dementia (LBD) is a progressive brain disorder in which Lewy bodies (abnormal deposits of a protein called alpha-synuclein) build up in areas of the brain that regulate behavior, cognition, and movement.
A complex disease, LBD can present with a range of symptoms including problems with thinking, memory, moving, sleep and/or changes in behavior, to name a few of the physical, cognitive, and behavioral symptoms.
LBD also affects autonomic body functions, such as blood pressure control, temperature regulation, and bladder and bowel function. Progressively debilitating, LBD can also cause people to experience visual hallucinations or act out their dreams.
LBD is an umbrella term for two closely related clinical diagnoses: Parkinson’s disease dementia and dementia with Lewy bodies (DLB).
The causes of LBD are not yet well understood, but research is ongoing in this area. There are probably multiple factors involved, including genetic and environmental risk factors that combine with natural aging processes to make someone susceptible to LBD.
This condition impairs thinking, such as memory, executive function (planning, processing information), or the ability to understand visual information. Patients with LBD may have fluctuations in attention or alertness; problems with movement including tremors, stiffness, slowness and difficulty walking; hallucinations; and alterations in sleep and behavior.
Come back tomorrow for Part II!
“Suicide is the second leading cause of death among young adults and for every youth suicide it is estimated that 100 to 200 others attempt suicide. Young adulthood is a time when many people experience significant stress from life transitions such as gaining more independence and responsibility when moving from home and beginning college or a career. That stress has been amplified by the COVID-19 pandemic. Yet, we’ve seen striking glimmers of resilience – the ability to bounce back from a negative experience or difficult challenge. ”
JED Foundation
“Leukemia is the most common cancer in children and teens, accounting for almost 1 out of 3 cancers. Most childhood leukemias are acute lymphocytic leukemia (ALL). Most of the remaining cases are acute myeloid leukemia (AML). Chronic leukemias are rare in children. ”
American Cancer Society
“Lymphoplasmacytic lymphoma (LPL) is a low-grade (slow-growing) non-Hodgkin lymphoma. It develops from B lymphocytes (a type of white blood cell) that become abnormal and grow out of control. The abnormal cells in LPL can produce large amounts of abnormal antibodies (sometimes called ‘paraprotein’). In most cases of LPL, this is an IgM abnormal antibody. LPL with IgM detectable on blood tests is called Waldenström’s macroglobulinaemia (WM). It is named after the scientist who first described it. All types of LPL are treated in the same way.”.
Lymphoma Action (https://lymphoma-action.org.uk)