Bite marks on the body are the first sign of a bug infestation.
However; there are many species of bloodsucking mites and insects some of which typically include fleas, lice, ticks, bed bugs and so on. So how can you tell what is biting you?
This article will inform you the differences between bed bug bites vs lice bites in order to help you better understand what is biting you.
The first sign of a bed bug infestation is bite marks on your body as well as those of your family members. However, in many people, there is no significant visible reaction as they may have grown immune to the bed bug bites. Hence; it is important to also watch out for other tell-tale signs of bed bugs which typically include brown or rust colored stains on mattresses, discarded white or brown colored shells, as well as an obnoxious almond like smell in the air near the sleeping areas.
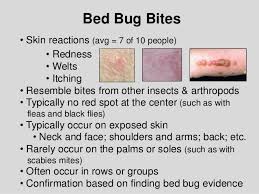
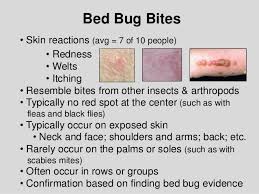
Bed bug bites also have following distinguishing characteristics:
- Bite marks may be seen on face, arms, legs and neck.
- The bites typically produce swollen bump with or without a red spot at the centre.
- The bites may be present in a linear pattern with groups of 2 or three bumps in one spot where the bed bug has inserted its mouthparts into the skin.
- In some people, the bites might lead to an allergic reaction which can cause intense itchiness, pain, and inflammation.
Bed bugs hide during the daytime and usually come out only at night-time to feed. So make sure you check your sleeping areas for bed bug signs. The pests also tend to hide in cracks and crevices around the bedding, so visually examine these areas. You will also have to vacuum the entire house and, if needed, discard heavily infested items.
Now Lice=What’s the actual difference with Beg Bugs?
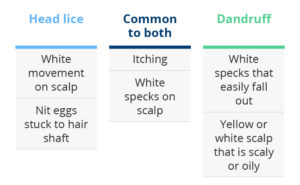
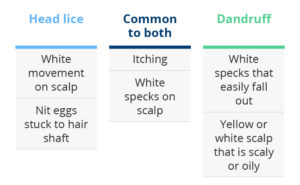
Body lice or head lice are common reasons why humans develop itchiness in their scalp or other body parts. The main similarity between bed bugs vs body lice is that both are typically seen in low economy housing areas or areas where humans have to live in close or cramped quarters under unsanitary conditions. Body lice are also common in school-aged children as they tend to come in close contact with infested kids. Bed bugs may be even found in the cleanest of places including five star hotels or posh residential areas. This is because; they have nothing to do with cleanliness or hygiene and usually come inside one’s homes through the luggage or even through buses, planes, movie theatres and retail stores.
Body lice bites can cause severe irritation on the skin. In sensitive people, red bumps might arise on the bitten areas. Large infestation can even lead to pain, fever, headaches and chills. Crab lice (pubic lice) often produce bluish spots about 1/10th of an inch in measurement in the bitten regions.
Summary of differences between bed bugs and body lice
- Bed bugs are larger in size than body or hair lice and can be best compared (in size as well as appearance) to an apple seed. Body lice or hair lice measure upto 3mm in length.
- Bed bugs leave characteristic tell-tale signs like a almond-like smell, discarded shells or exoskeletons as well as bloody or fecal matter on the bedding and sleeping areas. Body lice are usually only found through combing with a fine toothed comb.
- Bed bugs get transported from place to place through infested hotels, planes, buses or trains etc. Body lice such as crab lice are transmitted through sexual activities.
- Bed bug bites vs body lice bites: The former may be seen on face, arms, back, neck, chest or other exposed body parts. Body lice or hair lice bites may be present only on specific areas such as scalp, pubic region etc.
- Bed bug bites do not lead to any diseases. Body lice can lead to shivering, fever, aches and pains, especially in case of more severe infestations.
- The best remedies for both bed bug bites and body lice bites is treating and eliminating the infestations from the root. Bed bug infestations might need an integrated pest control approach such as vacuuming, discarding infested items, and spraying or dusting the areas with bed bug products. In case of lice, one will need to use lice combs, anti-lice solutions, lotions, shampoos and soaps to kill the larvae and eggs.
Though potentially harmless, both bed bug bites and body lice bites can be extremely annoying and itchy. Hence, it is vital to know how to identify the bug bites VS. lice through how they feel and look in order to seek proper medical attention or treat it at home so you get rid of the entire infestation of bed bugs or lice.