More than 65 million Americans overall have asthma and allergies. Some people may have one or both of these conditions. About 25 million Americans have asthma (20 million adults and 5 million children) About 32 million Americans have food allergies (26 million adults and 6 million children). About 24 million Americans have rhinitis (hay fever), or nasal allergies (19.2 million adults and 5.2 million children) There is no cure for asthma or allergies.
Rates of asthma are highest among African Americans and Puerto Ricans, young boys, and people living below the poverty line. Each year, asthma leads to more than 1.6 million emergency department visits and 170,000 hospital stays. For many, the change in seasons—with more allergens in the environment—can increase wheezing, chest tightness, shortness of breath, coughing, or severe asthma attacks.
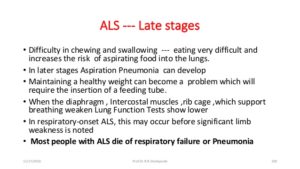
Asthma is a chronic (long-term) condition that affects the airways in the lungs. The airways are tubes that carry air in and out of your lungs. If you have asthma, the airways can become inflamed and narrowed at times. This makes it harder for air to flow out of your airways when you breathe out. Many of those affected with Covid 19 with asthma have a harder time with dealing with it compared to those with no asthma due to the condition affecting breathing to begin with.
Normally, the body’s immune system helps fight infections. But it may also respond to other things you breathe in, such as pollen or mold. These are things that trigger symptoms of asthma to come on. In some people, the immune system reacts strongly by creating inflation. Ending result is the airways narrow causing it more difficult to breath. Over time, the airway walls can become thicker again making oxygen and carbon dioxide exchange not be as effective as someone without asthma.
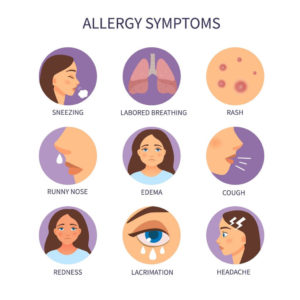
Symptoms of asthma may include:
- Chest tightness
- Coughing, especially at night or early morning
- Shortness of breath
- Wheezing, which is a whistling sound when you breathe out
Other conditions can cause these symptoms. but in asthma, the symptoms often follow a pattern:
- They come and go over time or within the same day.
- They start or get worse with viral infections, such as a cold.
- They are triggered by exercise, allergies, cold air, or breathing too fast from laughing or crying.
- They are worse at night or in the morning.
About 1 in 13 people in the United States has asthma, according to the Centers for Disease Control and Prevention external link . It affects people of all ages and often starts during childhood. Certain things can set off or worsen asthma symptoms, such as pollen, exercise, viral infections, or cold air. These are called asthma triggers. When symptoms get worse, it is called an asthma attack.
There is no cure for asthma, but treatment and an asthma action plan can help you manage it.
ALLERGY MONTH TOO:
Seasonal allergies often get lumped into one category. However, each season has its own unique allergens. Follow the guide below to see which months you can expect to see a flare up of which allergens.
For spring allergy sufferers, the joys of warmer weather, birds chirping and flowers blooming come at a price. Bothersome nose and eye symptoms, breathing difficulties and skin allergies can set in as trees begin to pollinate. Tree pollen season occurs between February and May.
Season length and timing varies each year depending on weather. Look at this winter this year how long it has lasted and finally spring has started this month. Due to a long, harsh winter, trees did not begin pollinating until March. Because pollen is microscopic, we cannot see it in the air and often do not know when the season has started until symptoms begin.
A common myth regarding spring allergies is that because symptoms often start in correlation with blooming flowers, the flower pollens contribute to the problem. Our allergies are due to plants that spread pollen by wind (anemophilous plants), which is how the pollen enters our eyes, noses, mouths or skin. These plants are not showy or eye-catching because they do not need to be. The plants we typically notice are usually flowering plants that are pretty for the purpose of catching the attention of pollinators like bees and other insects. These plant pollens are spread from plant to plant by the insects that visit them (entomophilous plants). For this reason, most of our pollen exposure is due to pollen in the air outdoors, and thus our allergies are to wind-pollinated plants.
Many trees are primarily pollinated by wind, and tree pollens are the main springtime allergen. Mold spores also contribute to spring allergies but are most bothersome in the fall. Common trees in the northwest Ohio region that contribute to allergy symptoms include oak, cottonwood, birch, maple, sycamore, ash, elm, hickory, walnut, beech and mulberry. There is limited cross-reactivity between tree pollens. This means that while some trees are related and pollens are somewhat similar, many tree pollens have unique features that prevent the ability to create a single treatment for tree pollen allergy. Allergists are specially trained physicians who can test patients to multiple different tree pollens and treat each patient uniquely for their specific tree pollen allergies.
For seasonal allergy sufferers, it is important to meet with a board-certified allergist to identify which allergens are most bothersome and to allow for more focused attention on avoidance measures and treatment options.