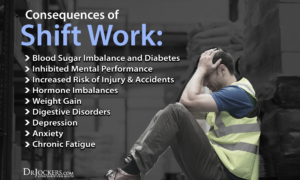
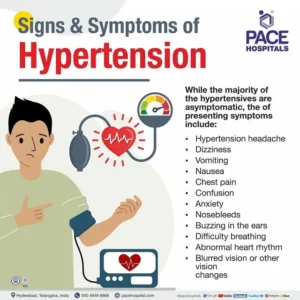
The signs and symptoms of high B/P=Hypertension could be:
- severe headaches.
- chest pain.
- dizziness.
- difficulty breathing.
- nausea.
- vomiting.
- blurred vision or other vision changes.
- anxiety.
Usually, high blood pressure causes no signs or symptoms. That’s why healthcare providers call it a “silent killer.” You could have high blood pressure for years and not know it. In fact, the World Health Organization estimates that 46% of adults with hypertension don’t know they have it.
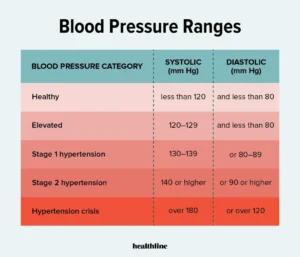
When your blood pressure is 180/120 mmHg or higher, you may experience symptoms like headaches, heart palpitations or nosebleeds. Blood pressure this high is a hypertensive crisis that requires immediate medical care.
Remember this, for many High blood pressure is known as the “silent killer” and its given that nickname for a reason. For those patients with high B/P they don’t feel ANY SIGNS OR SYMPTOMS OF HIGH B/P to go to the doctor! So they let their B/P get so high, never going to the MD or regularly checking their B/P on their own and puff they die awake or in their sleep due to the high B/P that caused the death!
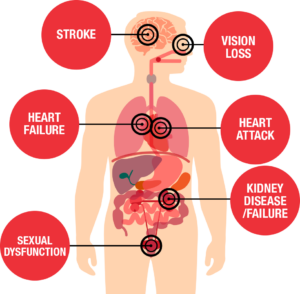
You may not feel that anything is wrong, but high blood pressure could be quietly causing damage that can threaten your health. The best prevention is knowing your numbers and making changes that matter in order to prevent and manage high blood pressure.
Why not just buy a blood pressure monitor from the pharmacy which will help you keep an eye on your B/P or even keeping your B/P therapeutic and have no HTN!
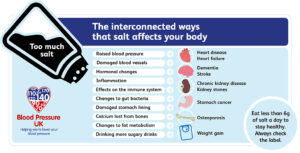
A BIG factor in helping to reduce or decrease high blood pressure for those with hypertension is DIET alone will impact greatly. Less SODIUM=Salt in the diet will have an impact in lowering your B/P!
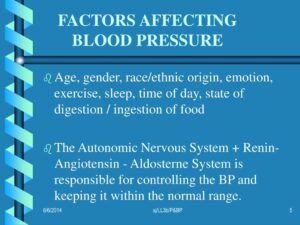
Your provider will diagnose you with one of two types of high blood pressure:
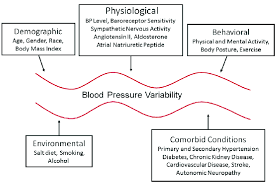
- Primary hypertension. Causes of this more common type of high blood pressure (about 90% of all adult cases in the U.S.) include aging and lifestyle factors like not getting enough exercise.
- Secondary hypertension. Causes of this type of high blood pressure include different medical conditions or a medication you’re taking.
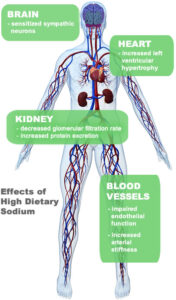
Most people with high b/p are asked to eat less sodium. Sodium attracts water and makes the body hold fluid. To pump the added fluid the heart works harder. Also sodium in the body causes the arteries to vasoconstrict increasing pressure in the vessels causing the pressure to rise.
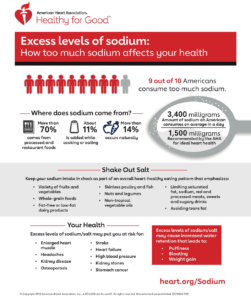
Most people with high b/p are asked to eat less sodium at 2000mg or less a day and this is to prevent water retention and vasoconstriction in which both actions increase the blood pressure. Follow your doctor’s advice about your sodium intake.
Many prepared foods and spices are high in sodium. But, the most common source of sodium is table salt. Table salt is 40% sodium and 60% chloride. One teaspoon of table salt contains 2000mg of sodium. Get rid of your table salt period will help you in trying to lower your B/P or keeping your B/P therapeutic (in the norm).
HINTS IN HOW TO LOWER YOUR SODIUM IN YOUR DIET:
What is Sodium (NA+)? One it’s an important substance in our body. It helps your body balance the level of fluid inside and outside of the cells; this prevents the cells from becoming dehydrated. To keep up this balance, the body needs about 2000mg of sodium a day or less. Yet most of us eat 3000 to 6000mg of sodium each day. On average Americans eat 3400mg of sodium a day and now it is recommended to eat 1500 mg a day. A major start is no salt shaker on the table and don’t add salt to your foods unless you know the amount in them already with not going over 1500 mg of salt a day or what your cardiologist recommends who is the expert!
Other tips could be:
-Season foods with fresh or dried herbs, vegetables, fruits or no-salt seasonings.
-Do not cook with salt or add salt to foods after they are on the table.
-Make your own breads, rolls, sauces, salad dressings, vegetable dishes and desserts when you can.
-Stay away from fast foods. They are almost all high in salt.
-Eat fresh, not frozen or canned, and do eat unsalted vegetables. These have less sodium than most processed foods. Read the labels and if they don’t have a label DON’T EAT IT. Read the labels and eat the portioned size it says to for 1 portion with keeping a diary of what you ate with adding the sodium and when it reached 2000mg no more food that day with salt in it unless the doctor prescribes less.
Know this frozen meals are often high in sodium. In fact, it’s estimated that around 70% of the sodium people consume in the United States comes from prepackaged, processed, and restaurant foods = high in sodium.
-Buy water packed tuna and salmon. Break it up into a bowl of cold water, and let stand for 3 minutes. Rinse, drain and squeeze out water.
-Don’t buy convenience foods such as prepared or skillet dinners, deli foods, cold cuts, hot dogs-one of the worst foods to eat to begin, frozen entrees or canned soups. These have lots of salt. Be picky on what you eat.
-Again, read all labels for salt, sodium or sodium products (such as sodium benzoate, MSG). Ingredients are listed in the order of amount used. A low sodium label means 140mg of less per serving. Try to buy products labeled low sodium/serving. Do not eat products that have more sodium than this per serving.
-AHA states, “If you drink, limit your alcohol consumption to no more than two drinks per day for men and no more than one drink per day for women. A drink is one 12 oz. beer, 4 oz. of wine, 1.5 oz. of 80-proof spirits or 1 oz. of 100-proof spirits.
I’ve read that red wine is heart healthy — can I drink as much as I’d like?
Unfortunately, red wine as a miracle drink for heart heath is a myth. The linkage reported in many of these studies may be due to other lifestyle factors rather than alcohol. Like any other dietary or lifestyle choice, it’s a matter of moderation and disciplining yourself in almost anything especially junk food, processed foods, foods high in fat or fried should once in awhile in aiding yourself in controlling your blood pressure. Don’t only do moderation when the B/P goes high instead make the moderate eating of bad foods a regular part of your life and high odds it will only aid in helping your B/P to stay normal or to get in a therapeutic range. The other way is only a high potential to aid in getting hypertension or increasing your b/p.
If you need help–
If cutting back on alcohol is hard for you to do on your own, ask your healthcare provider about getting help.
The AHA says your lifestyle plays an important role in treating your high blood pressure. If you successfully control your blood pressure with a healthy lifestyle, you might avoid, delay or reduce the need for medication.
Foods to keep out of your diet or ever have on a regular basis and have maybe have once every 3 months or less
-Canned Vegetables, sauerkraut. Self rising flour and corn meal. Prepared mixes (waffle, pancake, muffin, cornbread, etc…)
-Dairy Products high in fat- like buttermilk (store-bought), canned milks unless diluted and used as regular milk). I personally switched to skim milk and drink it every day and with other things taken in my life in moderation with trying to watch my weight still keeps my b/p under 120/80. Egg substitute limit to ½ cup/day. Eggnog (store bought) and salted butter or margarine do not buy everyday but have eggnog around holiday time is what I do and that’s it. I limit my butter intake where it is on bread and never add it to cooking or have extra on the table for like mashed potatoes. Trust me processed foods have plenty in them and bakery goods without question.
-Soups: Boullon (all kinds), canned broth, dry soup mixes, canned soups are severely high in sodium especially the noodles you add water to. Just have one of them and your already over 1000mg of salt. Surprise, Dietary Guidelines for Americans recommends adults limit sodium intake to less than 2,300 mg per day—that’s equal to about 1 teaspoon of table salt! Salt is in the majority of foods so look on the back of the food and read the amount of fat,carbohydrates and salt is in a serving with seeing what the food’s size of a serving is. It may make you fall in the chair.
-Meats and meat substitutes not to buy=Canned meats, canned fish, cured meats, all types of sausages, sandwich meats, peanut butter, salted nuts. High in sodium again.
-Prepared mixes (pie, pudding, cake) or store bought pies, cakes, muffins.
-Cooking ingredients to use low sodium type or limit to 2 tbsp/day=ketchsup, chili sauce, barbecue sauce, mustard, salad dressing. Read the label!
-Drinks to stay away from Athletic Drinks (such as energy drinks-caffeine/Gatorade), canned tomato or vegetable juice (unless unsalted). Caffeine is a commonly used neurostimulant that also produces cerebral vasoconstriction by antagonizing adenosine receptors. Chronic caffeine use results in an adaptation of the vascular adenosine receptor system presumably to compensate for the vasoconstrictive effects of caffeine=vasoconstriction of all blood vessels=this increases your b/p.
NIH=The National Library of Meidicine found this with caffeine (https://www.ncbi.nlm.nih.gov/books/NBK202224/):
The West Florida Vein Center states this about caffeine:
“Caffeine is a drug found in coffee, soda and tea, doesn’t just wake you up. It sets your whole body into a different motion, stimulating the nervous system and constricting blood vessels. Caffeine is safe when ingested in moderation, but excessive consumption can lead to vascular complications like high blood pressure, poor circulation and narrow blood vessels. I have 2 cups a day on average. Being a night RN I have one in the morning to have one at night. When off of work just one or two in the am.
Upon consumption, caffeine gives you your morning jolt of energy. It achieves this by attaching to your adenosine receptors, which ordinarily dilate your brain’s blood vessels. Instead, your blood vessels constrict, also known as vasoconstriction. When vasoconstriction of the brain occurs, the pituitary gland sounds an alarm and reacts as if in an emergency state. It then releases adrenaline, which leads to increased heart rate.“
Know adrenaline is released in fight or flight and adrenaline causes peripheral vasoconstriction which further increases the B/P due to pressure build up in the vessels away from the core or center of the body. That is what peripheral means.
The West Florida Vein Center further states:
“With vasoconstriction comes faster heart rate but slower blood flow. A study by “Human Brain Mapping” found heavy caffeine users experienced “reduced cerebral blood flow by an average of 27 percent.” What this means? Excessive caffeine intake leads to unnecessary stress on your venous system. Because your brain receives an inadequate amount of blood, your whole venous system operates under stress to compensate for the blood flow changes.
When stressed, veins are at greater risk of disease. Venous conditions like varicose veins and deep vein thrombosis can occur with vasoconstriction. Narrow blood vessels can prevent sufficient blood flow, causing clotting and inflammation. To avoid stressing your venous system, limit coffee intake to 24 ounces per day.” OR we say less if you can! Even better is decaffeinated coffee and no venous constriction will occur or if you need the caffeine have one glass or 12 ounces of caffeinated and the rest of the day decaffeinated coffee.
So yes, long term caffeine heavy users do get overall VASOCONSTRICTION that increases your blood pressure in the body, including in the brain. While there’s no broad percentage of caffeine dependence in the US population, smaller studies have been conducted. According to a study conducted by the University of Florida, 28% fulfilled the criteria for caffeine dependence compared to 50% for alcohol and 80% for nicotine. From this study 2 factors cause vasoconstriction Nicotine and Caffeine. Remember one of the symptoms of high B/P is a headache! So change your diet if you need to in your life, based on this information and hope it is useful!
Remember Moderation to stopping completely out of your diet things that increase your blood pressure is the key to helping you reach normal blood pressure with other factors like obesity, and disease from Diabetes to Athero- sclerosis (which is partly or completely blocking an artery vessel) including arteriosclerosis which is brittle arteries and Renal Failure (acute or chronic).
(Updated 5/12/24)


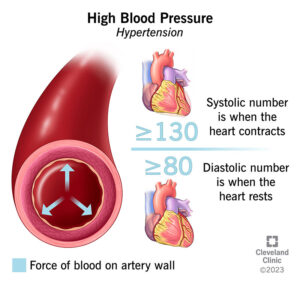
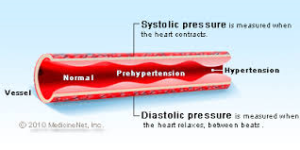 Systolic BP is heart at work, Diastolic BP is heart at rest!
Systolic BP is heart at work, Diastolic BP is heart at rest!