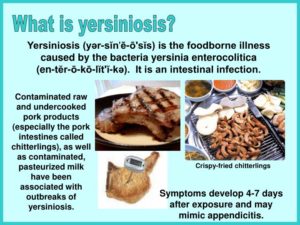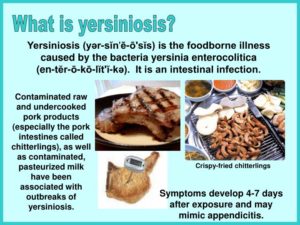
Yersiniosis is an infection caused most often by eating raw or undercooked pork contaminated with Yersinia enterocolitica bacteria. CDC estimates Y. enterocolitica causes almost 117,000 illnesses, 640 hospitalizations, and 35 deaths in the United States every year. Children are infected more often than adults, and the infection is more common in the winter.
Yersinia are bacteria that can cause illnesses in humans.
Yersiniosis refers to the illnesses caused by Y. enterocolitica and less often by Y. pseudotuberculosis infections.
Y. enterolitica are the most common species causing human enteric (intestinal) yersiniosis.
Pigs are the major animal reservoir for the few strains of Y. enterocolitica that cause human illness, but rodents, rabbits, sheep, cattle, horses, dogs, and cats also can carry strains that cause human illness.
The Symptoms:
The symptoms of yersiniosis depend on the age of the person infected. Infection occurs most often in young children. Common symptoms in children are fever, abdominal pain, and diarrhea, which is often bloody. Symptoms typically develop 4 to 7 days after exposure and may last 1 to 3 weeks or longer. In older children and adults, right-sided abdominal pain and fever may be the predominant symptoms and may be confused with appendicitis. Complications are rare, and may include skin rash, joint pains, or spread of bacteria to the bloodstream.
CDC estimates that infections with Yersinia enterocolitica cause almost 117,000 illnesses, 640 hospitalizations, and 35 deaths in the United States every year. Children are infected more often than adults, and the infection is more common in the winter.
How Humans get this illness:
Most people become infected by eating contaminated food, especially raw or undercooked pork, or through contact with a person who has prepared a pork product, such as chitlins. For example, babies and infants can be infected if their caretakers handle contaminated food and then do not wash their hands properly before handling the child or the child’s toys, bottles, or pacifiers.
People occasionally become infected after drinking contaminated milk or untreated water, or after contact with infected animals or their feces.
On rare occasions, people become infected through person-to-person contact. For example, caretakers can become infected if they do not wash their hands properly after changing the diaper of a child with yersiniosis.
Even more rarely, people may become infected through contaminated blood during a transfusion.
How this illness is diagnosed:
Yersiniosis usually is diagnosed by detecting the bacteria in the stool of an infected person. Many laboratories do not routinely test for Yersinia, so it is important that the clinician notifies the laboratory when yersiniosis is suspected so that special tests can be done.
The long-term consequences of yersiniosis:
Most symptoms go away completely. However, some people may experience the following:
- Joint pain, called reactive arthritis, most commonly in the knees, ankles, or wrists. These joint pains usually develop about 1 month after yersiniosis illness begins and generally go away after 1 to 6 months.
- A skin rash, called “erythema nodosum,” on the legs and torso. The rash is more common in women and usually goes away within a month.
How you can protect yourself and the family from this infection?
- Avoid eating raw or undercooked pork.
- Consume only pasteurized milk and milk products, such as soft cheese, ice cream, and yogurt.
- Wash hands thoroughly with soap and water before eating and preparing food, especially touching raw meat.
- After handling raw chitlins, clean hands and fingernails carefully with soap and water before touching infants or their toys, bottles, or pacifiers. Someone other than the person handling food should care for children while chitlins are being prepared.
- Prevent cross-contamination in the kitchen by using one cutting board for raw meat and another cutting board for fresh produce. Carefully clean all cutting boards, countertops, and utensils with soap and hot water after preparing raw meat.
- Dispose of animal feces (poop) in a sanitary manner.
Treatment:
1-Care in patients with this illness infection is primarily supportive, with good nutrition and hydration being mainstays of treatment.
2-First-line drugs used against the bacterium include aminoglycosides and trimethoprim-sulfamethoxazole (TMP-SMZ). Other effective drugs include third-generation cephalosporins, tetracyclines (not recommended in children under 8 y), and fluoroquinolones (not approved for use in children under 18 y).