Cancer seems like a thunder bolt that it all of a sudden hits us from nowhere, like what happened to my Dad that was in 1999 when he was diagnosed with pancreatic cancer with passing on in about 6 months after diagnosed. Than the hit from nowhere makes the patient and significant others suddenly crippled and not prepared for this diagnosis (facing it with little knowledge or in some cases nothing you can do for the patient since its fatal other than support). No wonder why cancer fears society. To top that alone it is costly, debilitating, depressing, and even fatal, like in my father’s case.
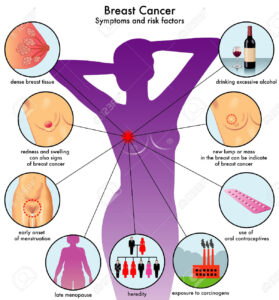
Early detection can vastly improve survival figures, that is not just pertaining to breast cancers but to most diseases period. Delaying to seek advice when changes are recognized is a big mistake.
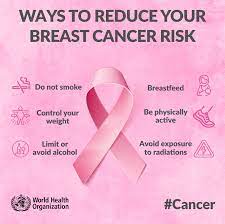
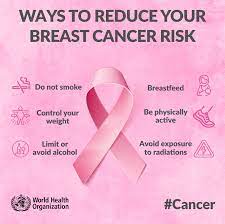
**Here are some general risk factors for cancer & try to prevent having them in your lives or abusing them (moderation – the key to many things that are not used that way in US). Abuse of anything results in disaster.
1.) Smoking (stop period) including chewing tobacco and dipping snuff. Best to stop these period.
The CDC states in 2020, an estimated 12.5% (30.8 million) of U.S. adults currently smoked cigarettes. Current cigarette smoking was defined as smoking ≥100 cigarettes during a lifetime and now smoking cigarettes either every day or some days.5
Lung cancer mainly occurs in older people. Most people diagnosed with lung cancer are 65 or older; a very small number of people diagnosed are younger than 45. The average age of people when diagnosed is about 70.
Lung cancer is by far the leading cause of cancer death , making up almost 25% of all cancer deaths. Each year, more people die of lung cancer than of colon, breast, and prostate cancers combined.
2.) Diets high in fat or low in fiber. Obesity as well is a risk factor for cancer, odds are high that the diet was high in fat even causing the obesity in the first place.
3.) Age is over 50 or too much unresolved stress in your life.
4.) Abuse of alcoholism or inadequate amount of vitamins or minerals in your diet. Exposure to environmental or occupational cancer causing substances (air, water, radiation, disaster like 9/11, or even food).
5.) Too much radiation from various sources (ex. Sun bathing to close to radiation treatments someone is receiving on a oncology unit, simply Sun overexposure).
6.) Fair complexion (pale) or even family history of cancers in the family (highest risk is within the nuclear family having a mother or father or sibling with cancer).
**Most cancers with heredity in the nuclear family including a bad life style puts that individual at higher probability of inheriting or getting that cancer.**
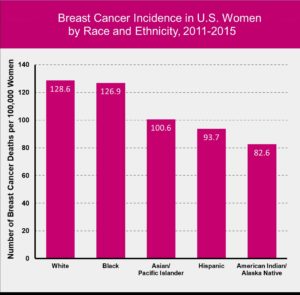
How ethnic groups play a part in breast cancer or any cancer:
Look at ethnicity; take a completely different country in eating alone. Let us look at Japan and their women. They eat a completely different diet than women in the USA. Japanese women have ¼ the amount of breast cancer than American women; is this mainly genetics? When Japanese women move to the great USA they assume our diets and get the same death rates from breast cancer that American women get when diagnosed with it. My eyes see diet in America (fast food=JUNK). Moderation if not completely banded out of your diet = fast food. Americans who eat junk food on a regular basis are looking at abusing fast food as oppose to a treating themselves to junk food now and than (this is what we call moderation).
Breastcancer.org states:
“Among younger women, Black and non-Hispanic Black women have higher rates of breast cancer compared to white and non-Hispanic white women. Among older women, white and non-Hispanic white women have higher rates of breast cancer compared to Black and non-Hispanic Black women.
White women are slightly more likely to develop breast cancer than Black, Hispanic, and Asian women. But Black women are more likely to develop more aggressive, more advanced-stage breast cancer that is diagnosed at a young age.
White women are slightly more likely to develop breast cancer than Black, Hispanic, and Asian women. But Black women are more likely to develop more aggressive, more advanced-stage breast cancer that is diagnosed at a young age. Black women are also more likely to die from breast cancer. Some of these differences in outcomes may be due to less access to mammography and lower quality medical care, as well as various lifestyle patterns (eating habits and weight issues for example) that are more common in some ethnic groups than in others. These factors can be changed and improved.
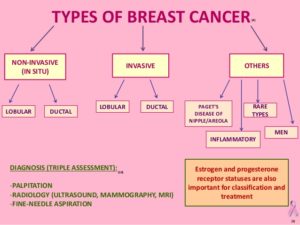
Still, triple-negative breast cancer, which is more aggressive than other types, is more common in Black women. Triple-negative breast cancer is estrogen-receptor-negative, progesterone-receptor-negative, and HER2-negative. New treatments for triple-negative breast cancer are being studied in clinical trials.”
The CDC states:
“What is already known about this topic? Breast cancer accounts for 30% of all cancers diagnosed in women.
What is added by this report? During 1999–2018, breast cancer incidence among women aged ≥20 years decreased an average of 0.3% per year, decreasing 2.1% per year during 1999–2004 and increasing 0.3% per year during 2004–2018. Incidence increased among start highlightnon-Hispanic Asian or Pacific end highlightIslander women and women aged 20–39 years but decreased among non-Hispanic White women and women aged 50–64 and ≥75 years.
What are the implications for public health practice? The U.S. Preventive Services Task Force currently recommends biennial mammography screening for women aged 50–74 years. Women aged 20–49 years might benefit from discussing potential breast cancer risk and ways to reduce risk with their health care providers.”
So what do we do at this point America or anywhere else?
We the people of America or anywhere can make the change in controlling many factors in our diet and exercise to control diseases period we have want to make the move and if we did disease decrease in time would be outstanding. In the end it would make our economy better with our insurance overall.
Ending line, this means less disease, less expense, and meaning better coverage (less out of our pockets financially). For this to even get started we the people in the USA have to be willing to alter diets and exercise to a healthy pattern not a junk food frequently diet or sedentary lifestyle. Help make America a better country for all citizens of all ages. Our government surely hasn’t helped us in prevention tactics to lower statistics in showing less breast cancer significantly.
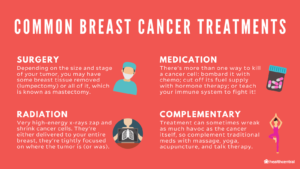
We do have many improvements with cancer treatment going from diagnostic tooling advancement with even drugs and drugs combined, a multitude of radiation methods and advanced surgical techniques. However, with all this due to increased cancer research, the government has yet to push the most important ingredient for cancer prevention. For every 3 dollars spent on cancer research, only one dollar goes spent in the area of prevention. When your government representative speaks of further cancer research you may want to find out is it for prevention or treatment. My vote is prevention before getting diagnosed with it. That is like the government waiting for a bomb to land on the USA before taking measures to prevent it. Why wait for the disaster when it can be prevented completely and no mess to deal with. Makes sense? Sure does to me and many.
Moderation with anything legal and not being abusive to your body, for ex. Alcohol or prescribed drugs, with the other modifiable factors you can change discussed yesterday, it simply takes someone with will power to make the change or one who already is doing the right activities with diet in their life had will power in doing this lifestyle. That is what it takes to prevent breast cancer and many other diseases simple means making changes in your life=willpower which includes a healthy diet, some regular exercising, keeping your weight ideal to your body mass index, and having the yearly physicals or addressing new symptoms by going to your doctor to have him or she evaluate what it is with the treatment for it. Obese? and can’t lose the weight on your own get a MD consult to see what surgery or other options you have to decrease weight. All it take is WILL POWER of that individual to do the right moves in life not to get cancer!
Instead of getting it wouldn’t you rather PREVENT it. Remember our disease killers in the USA. Our #1 killer is cardiovascular our #2 killer is cancer in America!
Ways to prevent breast cancer:

020414SMcC2244
The BEST way to go is not to ever get the cancer!!!
FIGHT BREAST CANCER AND EVEN DISEASE OVERALL BY PREVENTION; that is the KEY!!!!