According to the Center for Disease Control (CDC )the 2014 Ebola epidemic is the largest in history, affecting in West Africa. One imported case from Liberia and associated locally acquired cases in healthcare workers have been documented. CDC and partners are taking precautions to prevent the further spread of Ebola within the United States. We should have taken action with making limitations a long time ago but again our government seems to worry about other countries more than our own or else we would not have this potential epidemic. Look at what is finally being doing in airports at least in New York regarding visitors coming from Africa, they are being checked for disease in someway, that should have started years ago with the increase or population into our country from people unfortunately in other countries with more disease due to less protection or action due to their economy and what they can afford. Yet, in the end our government needs to protect us the US citizens and have a regulation much more tighter than it was if US citizens for whatever the reason is leaving this country to other countries for business (EX. News Report Employees.) or vacation is allowed; which it has been going on for ages. The key factor like to almost any disease or infection in or out of hospitals is: Prevention!
Share Compartment
MSF (Médecins Sans Frontières) health staff in protective clothing constructing perimeter for isolation ward.
***Background of the disease Ebola
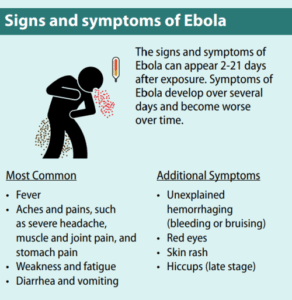
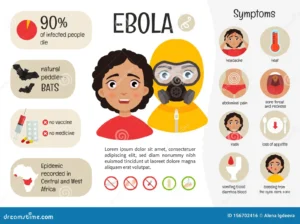
***The Ebola virus causes an acute, serious illness which is often fatal if untreated. Ebola virus disease (EVD) first appeared in 1976 in 2 simultaneous outbreaks, one in Nzara, Sudan, and the other in Yambuku, Democratic Republic of Congo. The latter occurred in a village near the Ebola River, from which the disease takes its name.
The past current outbreak in West Africa, (first cases notified in March 2014), is the largest and most complex Ebola outbreak since the Ebola virus was first discovered in 1976. There have been more cases and deaths in this outbreak than all others combined. It has also spread between countries starting in Guinea then spreading across land borders to Sierra Leone and Liberia, by air (1 traveller only) to Nigeria, and by land (1 traveller) to Senegal. God willing we do something fast enough with all the medical technology we have in America and fine a way to control it in our own country; we came through in controlling the flu and so many other epidemics.
The most severely affected countries, Guinea, Sierra Leone and Liberia have very weak health systems, lacking human and infrastructural resources, having only recently emerged from long periods of conflict and instability. On August 8, the WHO Director-General declared this outbreak a Public Health Emergency of International Concern. Well the US better do something fast to prevent both me and many others in this home land to keep us safe. By the way I am RN 26 years and this topic Ebola concerns me terribly.
PRESENTLY NOW according to the CDC this is the case with Ebola since this past Monday, “there are about 8,900 cases of Ebola infection worldwide with almost 4,500 deaths as of this week. And, the World Health Organization announced on Monday that we may see 10,000 new cases per week by December. Yes, that headline-making virus has now also made its way to the U.S. But, no, you will still probably not get it. Here’s what we know, and what you need to know about today’s Ebola situation.”
Transmission of Ebola
It is thought that fruit bats of the Pteropodidae family are natural Ebola virus hosts. Ebola is introduced into the human population through close contact with the blood, secretions, organs or other bodily fluids of infected animals such as chimpanzees, gorillas, fruit bats, monkeys, forest antelope and porcupines found ill or dead or in the rainforest that picked up this virus.
Ebola then spreads through human-to-human transmission via direct contact (through broken skin or mucous membranes) with the blood, secretions, organs or other bodily fluids of infected people, and with surfaces and materials (e.g. bedding, clothing) contaminated with these fluids.
Health-care workers have frequently been infected while treating patients with suspected or confirmed EVD. This has occurred through close contact with patients when infection control precautions are not strictly practiced or taught to the medical workers through detailed and concise information with written instructions, proper demonstration, with most important follow up by health care worker superiors like managers to nursing education depts.
For further information on this go to my reference http://www.who.int/mediacentre/factsheets/fs103/en/The World Health Organization. *** There is no FDA-approved vaccine available for Ebola, unfortunately but like most after damage occurs in enough quantities (which is the case) in time most diseases come up with one regarding the many over the few diseases we haven’t seem to have invented yet. So the key for this disease right now is PREVENTION of it.
Keep in mind through the CDC we are in the U.S. working on a treatment. Let us take a look.
“Experimental vaccines and treatments for Ebola are under development, but they have not yet been fully tested for safety or effectiveness.
Recovery from Ebola depends on good supportive care and the patient’s immune response. People who recover from Ebola infection develop antibodies that last for at least 10 years, possibly longer. It isn’t known if people who recover are immune for life or if they can become infected with a different species of Ebola. Some people who have recovered from Ebola have developed long-term complications, such as joint and vision problems.”
Here are some tips given by the CDC (Center for Disease Control): If you travel to or are in an area affected by an Ebola outbreak, make sure to do the following:
- Practice careful hygiene. For example, wash your hands with soap and water or an alcohol-based hand sanitizer and avoid contact with blood and body fluids.
- Do not handle items that may have come in contact with an infected person’s blood or body fluids (such as clothes, bedding, needles, and medical equipment). In a hospital patients with contaminating diseases through blood, secretions or fluids of the body is when contact isolation is used to prevent the spread of diseases (EX. MRSA, VRE)that can be spread through contact with open wounds, urine, blood, simple secretions of the body (even tears or fluids coming from the eye). Health care workers making contact with a patient on contact isolation are required to wear gloves, a gown, even a mask if one wants (which I without question do for any contact isolation a pt is on for their contaminating disease to prevent spread on me or others). With Ebola it may even go into further restrictions with disease to PREVENT further contamination which is only watching the safety of all citizens and visitors in this country or hopefully this will be carried out in Africa and anywhere else at this point.
- Avoid funeral or burial rituals that require handling the body of someone who has died from Ebola.
- Avoid contact with bats and nonhuman primates or blood, fluids, and raw meat prepared from these animals.
- Avoid hospitals in West Africa where Ebola patients are being treated, if .not needed. The U.S. embassy or consulate is often able to provide advice on facilities.
Lets look at what has happened so far. Thomas Eric Duncan contracted the virus while in West Africa. He then flew on a commercial flight to visit family in the States in late September. On the 26th, he went to Texas Presbyterian Health Hospital with a fever and was sent home with Tylenol and antibiotics. Two days later, Duncan went back to the hospital, and on the 29th he was confirmed to be the first person diagnosed with Ebola on U.S. soil. He died on October 8th. He is one of three confirmed Ebola cases to be diagnosed in the U.S. The other two are nurses who were treating Duncan at the hospital. The first was Nina Pham, who is reportedly in “good condition.” The second, Amber Vinson, took a commercial airline flight back from Cleveland the day before developing a severe fever. While we don’t know if she was contagious on the flight, the CDC says she had a low-grade fever before boarding and it is in the processes of reaching out to other passengers on the flight. Check out part 2 tomorrow!





 10Years Ago
10Years Ago