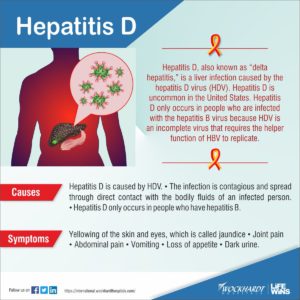
HEPATITIS D:
Hepatitis D (hepatitis delta) is a disease caused by the hepatitis D virus (HDV), a small circular enveloped RNA virus. This is one of five known hepatitis viruses: A, B, C, D, and E. HDV is considered to be a sub-viral satellite because it can propagate only in the presence of the hepatitis B virus (HBV).
How its transmitted:
Transmission of HDV can occur either be via simultaneous infection with HBV (coinfection) or superimposed on chronic hepatitis B or hepatitis B carrier state (superinfection).
Both superinfection and coinfection with HDV results in more severe complications compared to infection with HBV alone. These complications include a greater likelihood of experiencing liver failure in acute infections and a rapid progression to liver cirrhosis, with an increased chance of developing liver cancer in chronic infections. In combination with hepatitis B virus, hepatitis D has the highest fatality rate of all the hepatitis infections, at 20%.
The routes of transmission of hepatitis D are similar to those for hepatitis B. Infection is largely restricted to persons at high risk of hepatitis B infection, particularly injecting drug users and persons receiving clotting factor concentrates. Worldwide more than 15 million people are co-infected. HDV is rare in most developed countries, and is mostly associated with intravenous drug use.
How its diagnosed:
HDV infection is diagnosed by high levels of anti-HDV immunoglobulin G (IgG) and immunoglobulin M (IgM), and confirmed by detection of HDV RNA in serum.
However, HDV diagnostics are not widely available and there is no standardization for HDV RNA assays, which are used for monitoring response to antiviral therapy.
How it’s treated:
The vaccine for hepatitis B protects against hepatitis D virus because of the latter’s dependence on the presence of hepatitis B virus for it to replicate.
Low quality evidence suggests that interferon alpha can be effective in reducing the severity of the infection and the effect of the disease during the time the drug is given, but the benefit generally stops when the drug is discontinued, indicating that it does not cure the disease. Interferon is effective only in ~20% of cases.
The drug myrcludex B, which inhibits virus entry into hepatocytes, is in clinical trials as of October 2015
Hepatitis E:
Hepatitis E infection is found worldwide and is common in low- and middle-income countries with limited access to essential water, sanitation, hygiene and health services.
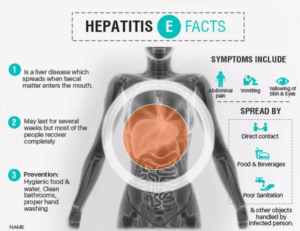
How it’s transmitted:
In these areas, the disease occurs both as outbreaks and as sporadic cases. The outbreaks usually follow periods of fecal contamination of drinking water supplies and may affect several hundred to several thousand persons. Some of these outbreaks have occurred in areas of conflict and humanitarian emergencies such as war zones and camps for refugees or internally displaced populations, where sanitation and safe water supply pose special challenges.
Sporadic cases are also believed to be related to contamination of water, albeit at a smaller scale. The cases in these areas are caused mostly by infection with genotype 1 virus, and much less frequently by genotype 2 virus.
In areas with better sanitation and water supply, hepatitis E infection is infrequent, with only occasional sporadic cases. Most of these cases are caused by genotype 3 virus and are triggered by infection with virus originating in animals, usually through ingestion of undercooked animal meat (including animal liver, particularly pork). These cases are not related to contamination of water or other foods.
How its diagnosed:
Definitive diagnosis of hepatitis E infection is usually based on the detection of specific anti-HEV immunoglobulin M (IgM) antibodies to the virus in a person’s blood; this is usually adequate in areas where the disease is common.
How it’s treated:
There is no specific antiviral therapy for acute hepatitis E. Physicians should offer supportive therapy. Patients are typically advised to rest, get adequate nutrition and fluids, avoid alcohol, and check with their physician before taking any medications that can damage the liver, especially acetaminophen. If any form of treatment, NIH NIDDK recommends this: “Treatment for acute hepatitis E includes resting, drinking plenty of liquids, and eating healthy foods to help relieve symptoms. Talk with your doctor before taking any prescription or over-the-counter medicines, vitamins or other dietary supplements NIH external link, or complementary or alternative NIH external link medicines—any of these could damage your liver. You should avoid alcohol until your doctor tells you that you have completely recovered from hepatitis E.”