Breast cancer is cancer that forms in the cells of the breasts.
After skin cancer, breast cancer is the most common cancer diagnosed in women in the United States. Breast cancer can occur in both men and women, but it’s far more common in women.
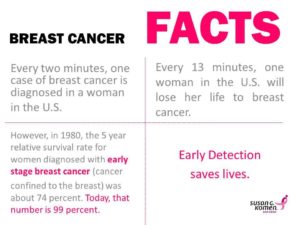
Public support for breast cancer awareness and research funding has helped improve the diagnosis and treatment of breast cancer. Breast cancer survival rates have increased, and the number of deaths has been declining, thanks to a number of factors such as earlier detection, new treatments and a better understanding of the disease.
Breast cancer prevention starts with healthy habits — such as limiting alcohol and staying physically active. Understand what you can do to reduce your breast cancer risk.
If you’re concerned about breast cancer, you may be wondering if there are steps you can take toward breast cancer prevention. Some risk factors, such as family history, can’t be changed. However, there are lifestyle changes you can make to lower your risk.
What can I do to reduce my risk of breast cancer?
Lifestyle changes have been shown in studies to decrease breast cancer risk even in high-risk women. The following are steps you can take to lower your risk:
- Limit alcohol. The more alcohol you drink, the greater your risk of developing breast cancer. If you choose to drink alcohol — including beer, wine or liquor — limit yourself to no more than one drink a day.
- Don’t smoke. Accumulating evidence suggests a link between smoking and breast cancer risk, particularly in premenopausal women. In addition, not smoking is one of the best things you can do for your overall health.
- Control your weight. Being overweight or obese increases the risk of breast cancer. This is especially true if obesity occurs later in life, particularly after menopause.
- Be physically active. Physical activity can help you maintain a healthy weight, which, in turn, helps prevent breast cancer. For most healthy adults, the Department of Health and Human Services recommends at least 150 minutes a week of moderate aerobic activity or 75 minutes of vigorous aerobic activity weekly, plus strength training at least twice a week.
- Breast-feed. Breast-feeding may play a role in breast cancer prevention. The longer you breast-feed, the greater the protective effect.
- Limit dose and duration of hormone therapy. Combination hormone therapy for more than three to five years increases the risk of breast cancer. If you’re taking hormone therapy for menopausal symptoms, ask your doctor about other options. You may be able to manage your symptoms with nonhormonal therapies, such as physical activity. If you decide that the benefits of short-term hormone therapy outweigh the risks, use the lowest dose that works for you.
- Avoid exposure to radiation and environmental pollution. Medical-imaging methods, such as computerized tomography, use high doses of radiation, which have been linked with breast cancer risk. Reduce your exposure by having such tests only when absolutely necessary. While more studies are needed, some research suggests a link between breast cancer and exposure to the chemicals found in some workplaces, gasoline fumes and vehicle exhaust.
Can a healthy diet prevent breast cancer?
Eating a diet rich in fruits and vegetables hasn’t been consistently shown to offer protection from breast cancer. In addition, a low-fat diet appears to offer only a slight reduction in the risk of breast cancer.
However, eating a healthy diet may decrease your risk of other types of cancer, as well as diabetes, heart disease and stroke. A healthy diet can also help you maintain a healthy weight — a key factor in breast cancer prevention.
Is there a link between birth control pills and breast cancer?
A number of older studies suggested that birth control pills slightly increased the risk of breast cancer, especially among younger women. In these studies, however, 10 years after discontinuing birth control pills women’s risk of breast cancer returned to the same level as that of women who never used oral contraceptives. Current evidence does not support an increase in breast cancer with birth control pills.
Be vigilant about breast cancer detection. If you notice any changes in your breasts, such as a new lump or skin changes, consult your doctor. Also, ask your doctor when to begin mammograms and other screenings.
Once you’ve been diagnosed with breast cancer, your doctor works to find out the specifics of your tumor. Using a tissue sample from your breast biopsy or using your tumor if you’ve already undergone surgery, your medical team determines your breast cancer type. This information helps your doctor decide which treatment options are most appropriate for you.
Here’s what’s used to determine your breast cancer type.
Is your cancer invasive or noninvasive?
Whether your cancer is invasive or noninvasive helps your doctor determine whether your cancer may have spread beyond your breast, which treatments are more appropriate for you, and your risk of developing cancer in the same breast or your other breast.
- Noninvasive (in situ) breast cancer. In situ breast cancer refers to cancer in which the cells have remained within their place of origin — they haven’t spread to breast tissue around the duct or lobule. One type of noninvasive cancer called ductal carcinoma in situ (DCIS) is considered a precancerous lesion. This means that if it were left in the body, DCIS could eventually develop into an invasive cancer. Another type of noninvasive cancer called lobular carcinoma in situ (LCIS) isn’t considered precancerous because it won’t eventually evolve into invasive cancer. LCIS does, however, increase the risk of cancer in both breasts.
- Invasive breast cancer. Invasive (infiltrating) breast cancers spread outside the membrane that lines a duct or lobule, invading the surrounding tissues. The cancer cells can then travel to other parts of your body, such as the lymph nodes. If your breast cancer is stage I, II, III or IV, you have invasive breast cancer.
In what part of the breast did your cancer begin?
The type of tissue where your breast cancer arises determines how the cancer behaves and what treatments are most effective. Parts of the breast where cancer begins include:
- Milk ducts. Ductal carcinoma is the most common type of breast cancer. This type of cancer forms in the lining of a milk duct within your breast. The ducts carry breast milk from the lobules, where it’s made, to the nipple.
- Milk-producing lobules. Lobular carcinoma starts in the lobules of the breast, where breast milk is produced. The lobules are connected to the ducts, which carry breast milk to the nipple.
- Connective tissues. Rarely breast cancer can begin in the connective tissue that’s made up of muscles, fat and blood vessels. Cancer that begins in the connective tissue is called sarcoma. Examples of sarcomas that can occur in the breast include phyllodes tumor and angiosarcoma.
FYI a complication that can occur with advanced cancer that many of you may be unaware of. Bone metastasis occurs when cancer cells spread from their original site to a location in the bone. The most common types of cancer more likely to spread to bone include breast, prostate and lung cancers.
Bone metastasis can occur in any bone, but more commonly occurs in the pelvis and spine. Bone metastasis may be the first sign that you have cancer, or it may occur years after your cancer treatment is completed, ex. Hodgkins Disease.
Signs and symptoms of bone metastasis may include the following:
- Bone pain (back and pelvic pain are most common)
- Unexplained broken bones
- Loss of urine and/or bowel function
- Weakness in the legs
- High levels of calcium in the blood (hypercalcemia), which can cause nausea, vomiting and confusion
The most common problem with metastatic bone cancer is pain and fractures. Metastatic bone cancer usually can’t be cured, but instead the goal is to provide pain relief and control further spread. Treatment can make a big difference and may include the following:
- Medications to repair and build new bone — These medications are similar to those used by people with osteoporosis and can help in building and strengthening your bone.
- Chemotherapy — Given as a pill or through a vein, used to control and treat cancer that has spread to the bone.
- Traditional radiation therapy — Radiation is given as external beam therapy to treat the cancer in the bone.
- Hormone therapy — Medications are used to block hormones (for breast and prostate cancers) that help control the spread of cancer to the bone.
- Surgery — Used to fix a fracture and stabilize a break from the cancer in the bone.
- Cryoablation — A special technique that freezes the cancer cells.
- Radiofrequency ablation — A special technique that heats the cancer cells.
- Chemoradiation — A form of internal radiation that is given through the vein and travels to the site of bone metastasis and targets the cancer cells.
- Pain medications — Medications provided with the goal of relieving and controlling pain from bone metastasis.
- Physical therapy — Exercises may be prescribed to assist in strengthening muscles and providing any assistive devices that may help you (cane, walker, crutches, etc.).
If you’re living with metastatic bone cancer, you may find help and resources from a website called Bone Health in Focus. It was established with partners including BreastCancer.org, the National Lung Cancer Partnership and Us TOO International Prostate Cancer Education & Support Network to offer resources that help patients and caregivers understand more about cancer that has spread to the bone (find the site at www.bonehealthinfocus.com).
Mayo Clinic information on cancer that has spread to the bone can be found at http://www.mayoclinic.org/diseases-conditions/bone-metastasis/basics/definition/con-20035450.
Are you living with cancer that has spread to the bone? Feel free to share your experiences with each other on the this blog striveforgoodhealth.com or on TheMayoclinic.org.
Make the changes in your lifestyles including diet if you want to prevent cancer, live long and have a productive life.
REFERENCE: Mayoclinic.org