What is high blood pressure?
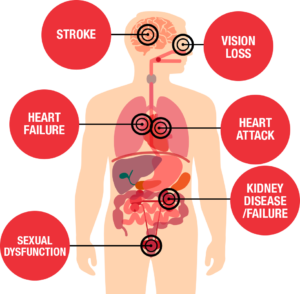
Blood pressure is the force of blood pushing against blood vessel walls as your heart pumps out blood. High blood pressure NIH external link, also called hypertension, is an increase in the amount of force that blood places on blood vessels as it moves through the body.
What are the kidneys and what do they do?
Healthy kidneys filter about a half cup of blood every minute, removing wastes and extra water to make urine. The urine flows from each kidney to the bladder through a pair of thin tubes called ureters, one on each side of your bladder. Your bladder stores urine. Your kidneys, ureters, and bladder are part of your urinary tract system.
How does high blood pressure affect the kidneys?
High blood pressure can constrict and narrow the blood vessels, which eventually damages and weakens them throughout the body, including in the kidneys. The narrowing reduces blood flow.
If your kidneys’ blood vessels are damaged, they may no longer work properly. When this happens, the kidneys are not able to remove all wastes and extra fluid from your body. Extra fluid in the blood vessels can raise your blood pressure even more, creating a dangerous cycle, and cause more damage leading to kidney failure.
How common are high blood pressure and kidney disease?
Almost 1 in 2 U.S. adults—or about 108 million people—have high blood pressure.1
More than 1 in 7 U.S. adults—or about 37 million people—may have chronic kidney disease (CKD).
High blood pressure is the second leading cause of kidney failure in the United States after diabetes, as illustrated in Figure 1.
Who is more likely to have high blood pressure or kidney disease?
High blood pressure
You are more likely to have high blood pressure if you
- are older. Blood pressures tends to increase with age. Our blood vessels naturally thicken and stiffen over time.
- have family members with high blood pressure. High blood pressure tends to run in families.
- have unhealthy lifestyle habits. Unhealthy habits such as eating too much sodium (salt), drinking too many alcoholic beverages, or not being physically active can increase your risk of high blood pressure.
- are African American. High blood pressure is more common in African American adults than in Caucasian, Hispanic, or Asian adults.
- are male. Men are more likely to develop high blood pressure before age 55; women are more likely to develop it after age 55.
Kidney disease
In addition to high blood pressure, other factors that increase your risk of kidney disease are
- diabetes
- a family history of kidney failure
- race or ethnicity—African Americans, Hispanics, and American Indians tend to have a greater risk for CKD
High blood pressure can be both a cause and a result of kidney disease.
What are the symptoms of high blood pressure and kidney disease?
Most people with high blood pressure do not have symptoms. In rare cases, high blood pressure can cause headaches.
Early CKD also may not have symptoms. As kidney disease gets worse, some people may have swelling, called edema. Edema happens when the kidneys cannot get rid of extra fluid and salt. Edema can occur in the legs, feet, ankles, or—less often—in the hands or face.
Symptoms of advanced kidney disease can include
- loss of appetite, nausea, or vomiting
- drowsiness, feeling tired, or sleep problems
- headaches or trouble concentrating
- increased or decreased urination
- generalized itching or numbness, dry skin, or darkened skin
- weight loss
- muscle cramps
- chest pain or shortness of breath
How do health care professionals diagnose high blood pressure and kidney disease?
High blood pressure
Blood pressure test results are written with the two numbers separated by a slash. The top number is called the systolic pressure and represents the pressure as the heart beats and pushes blood through the blood vessels. The bottom number is called the diastolic pressure and represents the pressure as blood vessels relax between heartbeats.
Your health care professional will diagnose you with high blood pressure if your blood pressure readings are consistently higher than 130/80 when tested repeatedly in a health care office.
Health care professionals measure blood pressure NIH external link with a blood pressure cuff. You can also buy a blood pressure cuff to monitor your blood pressure at home.

Kidney disease
To check for kidney disease, health care professionals use
- a blood test that checks how well your kidneys are filtering your blood, called GFR, which stands for glomerular filtration rate.
- a urine test to check for albumin. Albumin is a protein that can pass into the urine when the kidneys are damaged.
If you have kidney disease, your health care professional will use the same two tests to monitor your kidney disease.
How can I prevent or slow the progression of kidney disease from high blood pressure?
The best way to slow or prevent kidney disease from high blood pressure is to take steps to lower your blood pressure. These steps include a combination of medicines and lifestyle changes, such as
- being physically active
- maintaining a healthy weight
- quitting smoking
- managing stress
- following a healthy diet, including less sodium (salt) intake
No matter what the cause of your kidney disease, high blood pressure can make your kidneys worse. If you have kidney disease, you should talk with your health care professional about your individual blood pressure goals and how often you should have your blood pressure checked.
Medicines
Medicines that lower blood pressure can also significantly slow the progression of kidney disease. Two types of blood pressure-lowering medications, angiotensin-converting enzyme (ACE) inhibitors and angiotensin receptor blockers (ARBs), may be effective in slowing the progression of kidney disease.
Many people require two or more medications to control their blood pressure. In addition to an ACE inhibitor or an ARB, a health care professional may prescribe a diuretic—a medication that helps the kidneys remove fluid from the blood—or other blood pressure medications NIH external link.
Physical activity
Regular physical activity can lower your blood pressure and reduce your chances of other health problems.
Aim for at least 150 minutes per week of moderate-intensity aerobic activity. These activities make your heart beat faster and may cause you to breathe harder. Start by trying to be active for at least 10 minutes at a time without breaks. You can count each 10-minute segment of activity toward your physical activity goal. Aerobic activities include
- biking (Don’t forget the helmet.)
- swimming
- brisk walking
- wheeling yourself in a wheelchair or engaging in activities that will support you such as chair aerobics

If you have concerns, a health care professional can provide information about how much and what kinds of activity are safe for you.
Body weight
If you are overweight or have obesity, aim to reduce your weight by 7 to 10 percent during the first year of treatment for high blood pressure. This amount of weight loss can lower your chance of developing health problems related to high blood pressure.
Body Mass Index (BMI) is the tool most commonly used to estimate and screen for overweight and obesity in adults. BMI is a measure based on your weight in relation to your height. Your BMI can tell if you are at a normal or healthy weight, are overweight, or have obesity.
- Normal or healthy weight. A person with a BMI of 18.5 to 24.9 is in the normal or healthy range.
- Overweight. A person with a BMI of 25 to 29.9 is considered overweight.
- Obesity. A person with a BMI of 30 to 39.9 is considered to have obesity.
- Extreme obesity. A person with a BMI of 40 or greater is considered to have extreme obesity.
Your goal should be a BMI lower than 25 to help keep your blood pressure under control.3
Smoking
If you smoke, you should quit. Smoking can damage blood vessels, raise the chance of developing high blood pressure, and worsen health problems related to high blood pressure.
If you have high blood pressure, talk with your health care professional about programs and products to help you quit smoking.
Stress
Learning how to manage stress, relax, and cope with problems can improve your emotional and physical health. Some activities that may help you reduce stress include
- being physically active
- practicing yoga NIH external link or tai chi NIH external link
- listening to music
- focusing on something calm or peaceful
- meditating NIH external link

How does eating, diet, and nutrition affect high blood pressure and kidney disease?
Following a healthy eating plan can help lower your blood pressure. Reducing the amount of sodium in your diet is an important part of any healthy eating plan. Your health care professional may recommend the Dietary Approaches to Stop Hypertension (DASH) eating plan NIH external link. DASH focuses on fruits, vegetables, whole grains, and other foods that are healthy for your heart and lower in sodium, which often comes from salt. The DASH eating plan
- is low in fat and cholesterol
- features fat-free or low-fat milk and dairy products, fish, poultry, and nuts
- suggests less red meat, sweets, added sugars, and sugar-containing beverages
- is rich in nutrients, protein, and fiber

A registered dietitian can help tailor your diet to your kidney disease. If you have congestive heart failure or edema, a diet low in sodium intake can help reduce edema and lower blood pressure. Reducing saturated fat and cholesterol can help control high levels of lipids, or fats, in the blood.
People with advanced kidney disease should speak with their health care professional about their diet.
What should I avoid eating if I have high blood pressure or kidney disease?
If you have kidney disease, avoid foods and beverages that are high in sodium NIH external link.
Additional steps you can take to meet your blood pressure goals may include eating heart-healthy and low-sodium meals, quitting smoking, being active, getting enough sleep, and taking your medicines as prescribed. You should also limit alcoholic drinks—no more than two per day for men and one per day for women—because consuming too many alcoholic beverages raises blood pressure.
In addition, a health care professional may recommend that you eat moderate or reduced amounts of protein.
Proteins break down into waste products that the kidneys filter from the blood. Eating more protein than your body needs may burden your kidneys and cause kidney function to decline faster. However, eating too little protein may lead to malnutrition, a condition that occurs when the body does not get enough nutrients.
If you have kidney disease and are on a restricted protein diet, a health care professional will use blood tests to monitor your nutrient levels.