Schnitzler syndrome is considered to be a rare disorder characterized by a monoclonal IgM protein and chronic urticaria that is associated with considerable morbidity. We hypothesized that the syndrome may be under-recognized and patients may be deprived of highly effective therapy in the form of anakinra (an interleukin-1 receptor antagonist=inhibits interleukin 1). This treatment controls the condition but does not cure it. Around 15% of people develop complications, but the condition generally does not shorten life
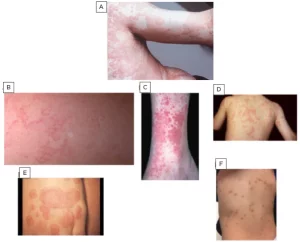
Schnitzler is a rare disease characterised by onset around middle age of chronic hives (urticaria) and periodic fever, bone pain and joint pain (sometimes with joint inflammation), weight loss, malaise, fatigue, swollen lymph glands and enlarged spleen and liver.
How its Diagnosed:
–Blood tests show a high concentration of specific gamma-globulins (monoclonal gammopathy) of the IgM type. It almost always has light chains of the κ-type. A variant in which IgG is raised has been described, which appears to be one-tenth as common.
–CBC, this could show signs of inflammation are often present: these include an increased white blood cell count (leukocytosis) and a raised erythrocyte sedimentation rate=we would see this in what we call a simple Complete Blood Count(CBC) and C-reactive protein blood test.
-There can be anemia of chronic disease showing low red blood count again in a simple CBC.
-Bone abnormalities can be seen on radiological imaging (often increased density or osteosclerosis)
-Biopsy
-What we call the Lipsker criteria require hives, the presence of monoclonal IgM, and at least 2 of the following: fever, joint pain or arthritis, bone pain, swollen lymph nodes, enlarged spleen or liver, elevated erythrocyte sedimentation rate, high levels of white blood cells, and findings of problems in bone imaging.
-What we call the Strasbourg criteria, the person must have hives and the presence of monoclonal IgM or IgG. Schnitzler’s is diagnosed if the person has IgM and two of the following, or IgG and three of the following: recurrent fevers, abnormalities in bone imaging, with or without bone pain, findings of neutrophil infiltration in a skin biopsy, high levels of white blood cells or C-reactive protein.
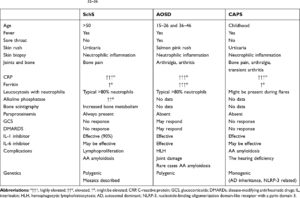
Other conditions which can cause periodic fevers, paraproteins or chronic hives that should be ruled out, include (and are not limited to) autoimmune or autoinflammatory disorders such as adult-onset Still’s disease, angioedema, hematological disorders such as lymphoma or monoclonal gammopathy of undetermined significance (MGUS), other causes of hives, cryoglobulinemia, mastocytosis, chronic neonatal onset multisystem inflammatory disease or Muckle–Wells syndrome.
Treatment:
As of 2017 no drug was approved to treat Schnitzlers. Drugs that inhibit interleukin 1 activity have been the preferred treatment since they emerged in 2005; since 2012 a consensus guideline has recommended treatment with anakinra. Immunosuppressant drugs such as corticosteroids, cyclooxygenase inhibitors, interferon alpha may be effective.