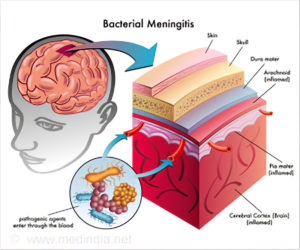
Meningococcal meningitis is a form of meningitis caused by a specific bacterium known as Neisseria meningitidis. Meningitis is characterized by inflammation of the membranes (meninges) around the brain or spinal cord. This inflammation can begin suddenly (acute) or develop gradually (subacute).
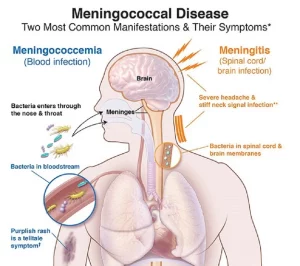
Meningococcal meningitis is a form of meningitis caused by a specific bacterium known as Neisseria meningitidis. Meningitis is characterized by inflammation of the membranes (meninges) around the brain or spinal cord. This inflammation can begin suddenly (acute) or develop gradually (subacute). Symptoms may include fever, headache, and a stiff neck, sometimes with aching muscles. Nausea, vomiting and other symptoms may also occur. Skin rashes occur in about half of all individuals with meningococcal meningitis.
Meningococcal meningitis is still associated with a high mortality rate and persistent neurological defects, particularly among infants and young children. Meningococcal meningitis without antibiotic therapy is uniformly fatal.
Meningococcal meningitis evolves when the bacteria, Neisseria meningitidis (N.meningitidis) progresses from initial adherence to the nasopharyngeal (nose and throat) mucosa to invasion of the deeper mucosal layers (the submucosa). These bacteria rapidly multiply, and can lead to a mild (subclinical) infection. However, in approximately 10-20% of cases, the N.meningitidis enters the bloodstream (meningococcemia). This systemic form of the disease, meningococcemia, usually precedes the development of meningococcal meningitis by 24-48 hours.
Key facts
- Meningitis is a devastating disease with a high case fatality rate and leading to serious long-term complications (sequelae).
- Meningitis remains a major global public-health challenge.
- Epidemics of meningitis are seen across the world, particularly in sub-Saharan Africa.
- Many organisms can cause meningitis including bacteria, viruses, fungi, and parasites.
- Bacterial meningitis is of particular concern. Around 1 in 10 people who get this type of meningitis die and 1 in 5 have severe complications.
- Safe affordable vaccines are the most effective way to deliver long-lasting protection
4 main causes of acute bacterial meningitis:
- Neisseria meningitidis (meningococcus)
- Streptococcus pneumoniae (pneumococcus)
- Haemophilus influenzae
- Streptococcus agalactiae (group B streptococcus)
The WHO World Health Organization states that these bacteria are responsible for more than half of the deaths from meningitis globally and they cause other severe diseases like sepsis and pneumonia; including other bacteria e.g., Mycobacterium tuberculosis, Salmonella, Listeria, Streptococcus and Staphylococcus, viruses such as enteroviruses and mumps, fungi especially Cryptococcus, and parasites like Amoeba are also important causes of meningitis.
Those at Risk:
Although meningitis affects all ages, young children are most at risk. Newborn babies are at most risk from Group B streptococcus, young children are at higher risk from meningococcus, pneumococcus and Haemophilus influenzae. Adolescents and young adults are at particular risk of meningococcal disease while the elderly are at particular risk of pneumococcal disease.
People all over the world are at risk of meningitis. The highest burden of disease is seen in a region of sub-Saharan Africa, known as the African Meningitis Belt, especially recognised to be at high risk of epidemics of meningococcal but also pneumococcal meningitis.
Higher risk is seen when people are living in close proximity, for example at mass gatherings, in refugee camps, in overcrowded households or in student, military and other occupational settings. Immune deficiencies such as HIV infection or complement deficiency, immunosuppression, and active or passive smoking can also raise the risk of different types of meningitis.