SARS, MERS, and Corona Viruses are all caused by some CORONA VIRUS!
Through the National Library of Medicine they state:
“In the 21st century, we have seen a total of three outbreaks by members of the coronavirus family. Although the first two outbreaks did not result in a pandemic, the third and the latest outbreak of Severe Acute Respiratory Syndrome Coronavirus 2 (SARS-CoV-2) culminated in a pandemic. This pandemic has been extremely significant on a social and international level. As these viruses belong to the same family, they are closely related. Despite their numerous similarities, they have slight distinctions that render them distinct from one another!”
Both COVID-19 and SARS are caused by coronaviruses. The virus that causes SARS is known as SARS-CoV, while the virus that causes COVID-19 is known as SARS-CoV-2. So what does this mean? A severe respiratory illness that is caused by a coronavirus (Severe acute respiratory syndrome-related virus of the genus Betacoronavirus)
SARS is caused by Betacoronavirus that is one of four genera of coronaviruses. Member viruses are enveloped, positive-strand RNA viruses that infect mammals, including humans. The first generation of covid.
COVID-19, which is caused by the 2019 coronavirus, has been dominate news starting 2019. However, you may have first become familiar with the term coronavirus during the severe acute respiratory syndrome (SARS) outbreak in 2003.
Both COVID-19 and SARS are caused by coronaviruses. The virus that causes SARS is known as SARS-CoV, while the virus that causes COVID-19 is known as SARS-CoV-2. There are also other types of human coronaviruses.
Despite similar names, there are several differences between the coronaviruses that cause COVID-19 and SARS.
“Abstract
Background: Middle East Respiratory Syndrome (MERS) is a viral respiratory illness that can spread from camels to people through direct physical . The MERS virus causes flu-like symptoms, with most patients developing pneumonia as a secondary infection. MERS is caused by a virus in the coronavirus family, and the syndrome is also called MERS-Coronavirus (MERS-CoV). MERS is passed primarily to people from infected camels.
Aims: To provide a review of the differences in pathogenesis, epidemiology and clinical features of COVID-19, SARS and MERS.
Sources: The most recent literature in the English language regarding COVID-19 has been reviewed, and extracted data have been compared with the current scientific evidence about SARS and MERS epidemics.
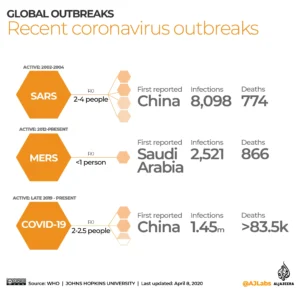
Content: COVID-19 seems not to be very different from SARS regarding its clinical features. The pathogenesis of human coronaviruses is mostly determined by viral particle binding to specific receptors rather than viremia. However, it has a fatality rate of 2.3%, lower than that of SARS (9.5%) and much lower than that of MERS (34.4%). The possibility cannot be excluded that because of the less severe clinical picture of COVID-19 it can spread in the community more easily than MERS and SARS. The actual basic reproductive number (R0) of COVID-19 (2.0-2.5) is still controversial. It is probably slightly higher than the R0 of SARS (1.7-1.9) and higher than that of MERS (<1). A gastrointestinal route of transmission for SARS-CoV-2, which has been assumed for SARS-CoV and MERS-CoV, cannot be ruled out and needs further investigation.
Implications: There is still much more to know about COVID-19, especially as concerns mortality and its capacity to spread on a pandemic level. Nonetheless, all of the lessons we learned in the past from the SARS and MERS epidemics are the best cultural weapons with which to face this new global threat since 2019 in China and 2020 in the USA.
Keywords: COVID-19; Coronavirus; Emerging infections; MERS; SARS.
Copyright © 2020 European Society of Clinical Microbiology and Infectious Diseases. Published by Elsevier Ltd. All rights reserved.”
Their references:
- PMID: 32234451
- PMCID: PMC7176926
- DOI: 10.1016/j.cmi.2020.03.026
Free PMC article
Middle East Respiratory Syndrome-MERS:
The MERS virus causes flu-like symptoms, with most patients developing pneumonia as a secondary infection. MERS is caused by a virus in the coronavirus family, and the syndrome is also called MERS-Coronavirus (MERS-CoV). MERS is passed primarily to people from infected camels. The first generation of Covid.
Key facts:
- Middle East respiratory syndrome (MERS) is a viral respiratory disease caused by Middle East respiratory syndrome coronavirus (MERS‐CoV) that was first identified in Saudi Arabia in 2012.
- Coronaviruses are a large family of viruses that can cause diseases ranging from the common cold to Severe acute respiratory syndrome (SARS), MERS and Coronavirus disease-2019 (COVID-19).
- Typical MERS symptoms include fever, cough and shortness of breath. Pneumonia is common, but MERS patients may not always develop this condition. Gastrointestinal symptoms, including diarrhoea, have also been reported among MERS patients.
- Approximately 35% of MERS cases reported to WHO have died.
- MERS-CoV is a zoonotic virus, meaning it is transmitted between animals and people. MERS-CoV has been identified and linked to human infections in dromedary camels in several Member States in the Middle East, Africa and South Asia.
- Human-to-human transmission is possible and has occurred predominantly among close contacts and in health care settings. Outside the health care setting, there has been limited human-to-human transmission.
Covid-19=Corona Virus Disease
This is the third serious Coronavirus outbreak that in less than 22 years, following SARS in 2002–2003 and MERS in 2012. While human strains of Coronavirus are associated with about 15% of cases of the common cold, the SARS-CoV-2 may present with varying degrees of severity, from flu-like symptoms to death. It is currently believed that this deadly Coronavirus strain originated from wild animals at the Huanan market in Wuhan, a city in Hubei province. Bats, snakes and pangolins have been cited as potential carriers based on the sequence homology of CoV isolated from these animals and the viral nucleic acids of the virus isolated from SARS-CoV-2 infected patients.
Extreme quarantine measures, including sealing off large cities, closing borders and confining people to their homes, were instituted in January 2020 to prevent spread of the virus, but by that time much of the damage had been done, as human-human transmission became evident.
The purpose for these measures are there are three primary ways to transmit the virus, including close person-to-person contact (droplet transmission), aerosol transmission, and transmission by touch=Purpose for mask, and if close to the patient with Covid-19 present gowns, gloves at least with the mask.
While these quarantine measures are necessary and have prevented a historical disaster along the lines of the Spanish flu, earlier recognition and earlier implementation of quarantine measures may have been even more effective. Lessons learned from SARS resulted in faster determination of the nucleic acid sequence and a more robust quarantine strategy. However, it is clear that finding an effective antiviral and developing a vaccine are still significant challenges.”
What’s the concern about COVID-19 variants? Are they more contagious?
Concern over variants, sometimes called strains, of the virus that causes COVID-19 is based on how the virus might change. A virus could get better at infecting people, spread faster or cause people to get sicker.
As a virus infects a group of people, the virus copies itself. During this process the genetic code can randomly change in each copy. These changes are called mutations.
Some mutations don’t have any effect on the virus.
But other mutations can:
- Make the virus better at infecting a person’s cells, causing serious illness.
- Make the virus better at avoiding the immune system.
- Cause tests for the virus to be less accurate.
- Cause vaccines to not work as well.
- Make medicine used to prevent or treat COVID-19 stop working or not work as well.
If a mutation changes how a virus acts in a group of people, it’s called a variant. Scientists across the world track the changes in the virus variants that cause COVID-19.
Omicron
The main variant in the United States is omicron. This variant spreads more easily than the original virus that causes COVID-19 and the delta variant. But omicron seems to cause less severe disease.
Omicron has a few major offshoots, also called sublineages. Together the omicron variants make up nearly all COVID-19 infections in the United States.
The Omicron variant, which emerged in November 2021, has many lineages. New lineages continue to emerge and spread in the United States and globally. We have the tools to fight variants. Take steps to protect yourself and others.
WHY SO MANY VACCINES FOR COVID-19?
First introduced in December 2020, the original COVID mRNA vaccines from both Pfizer and Moderna protected against the original SARS-CoV-2 virus.
Than with continuing to study COVID – 19 with people infected with it we came across the Omicron variant/strain.
The vaccines were replaced in September 2022 by “bivalent” vaccines, which targeted both the original virus and Omicron variants BA.4 and BA.5 to control the spread of COVID-19 to prevent another epidemic.
This is why so many vaccines; which many people are resistive to get to their reason in not understanding why the vaccines were pushed with not knowing about the logic behind the different variants needing a new vaccine to kill it!