Pacemakers are sometimes recommended for people with conditions that cause the heart to beat abnormally.
Each time the heart beats, the heart muscle contracts (pulls inwards) in preparation for pumping blood around the body.
The contractions are triggered by electrical pulses. These are generated by a group of specialised cells known as the sinoatrial node (SA node).
The SA node is often referred to as a natural pacemaker because it generates a series of electrical pulses at regular intervals.
The pulse is then sent to a group of cells known as the atrioventricular node (AV node). The AV node relays the pulse to the 2 lower chambers of the heart (the ventricles).
A pacemaker or implantable cardioverter defibrillator (ICD) is needed when something disrupts this process and causes an abnormal heartbeat.
An abnormal heartbeat is called an arrhythmia. Here are some of the most common causes of arrhythmias:
Sick sinus syndrome
In sick sinus syndrome, the SA node doesn’t work as it should. This can lead to an abnormally slow heartbeat (bradycardia), an abnormally fast heartbeat (tachycardia), or a combination of both.
Symptoms of sick sinus syndrome can include:
- a slower pulse than normal (bradycardia)
- extreme tiredness (fatigue)
- fainting (or nearly fainting)
- dizziness or lightheadedness
- shortness of breath
- chest pain
- irregular or fluttering heartbeats (palpitations)
Most cases of sick sinus syndrome are thought to be related to age.
Over time, the SA node tissue can become hardened and scarred. This can disrupt the normal pattern of electrical pulses released by the SA node.
Some types of medication can also trigger sick sinus syndrome as a side effect. These include calcium channel blockers and beta blockers.
Atrial fibrillation
Atrial fibrillation is a condition that causes the heart to beat abnormally fast.
This is usually considerably higher than 100 beats a minute (often 140 beats a minute or more).
Atrial fibrillation can usually be treated with medication, but some people don’t respond to treatment, so a pacemaker may be recommended.
Sometimes people with atrial fibrillation can have a much slower pulse rate than normal, which can also be intermittent (not continuous).
In these cases, a pacemaker will usually be recommended.
Heart block
In people with heart block, the pulse that needs to be sent from the SA node to the AV node is either delayed or absent.
Heart block can be caused when the heart is damaged (acquired heart block), or it can occur if a baby is born with 1 or more defects that affect their heart (congenital heart block).
If you have heart block and it’s causing troublesome symptoms, a pacemaker will usually be recommended.
Cardiac arrest
An implantable cardioverter defibrillator (ICD), which is a device similar to a pacemaker, is mainly used to prevent cardiac arrest.
A cardiac arrest is a potentially fatal condition where the electrical activity that controls the heart becomes so disrupted that the heart stops beating.
Unless it’s treated quickly, a cardiac arrest will be fatal.
An ICD can detect abnormal electrical signals that could indicate that a cardiac arrest is about to happen.
If the ICD detects these type of signals, it sends a powerful electrical shock to the heart.
This basically “reboots” the heart. After the shock, the heart should start beating normally again.
An ICD implantation may be recommended if you have had a cardiac arrest in the past or it’s thought you have a significant risk of having one in the future.
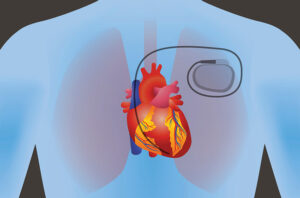
What are pacemakers?
Pacemakers are electronic devices that stimulate the heart with electrical impulses to maintain or restore a normal heartbeat. In 1952, Zoll described an effective means of supporting the patients with intrinsic cardiac pacemaker activity and/or conducting tissue by an artificial, electric, external pacemaker. The pacing of the heart was accomplished by subcutaneous electrodes but could be maintained only for a short period. In 1957, complete heart block was treated using electrodes directly attached to the heart. These early observations instilled the idea that cardiac electrical failure can be controlled. It ultimately led to the development of totally implantable pacemaker by Chardack, Gage, and Greatbatch. Since then, there have been several advancements in the pacemakers, and the modern-day permanent pacemaker is subcutaneously placed device.
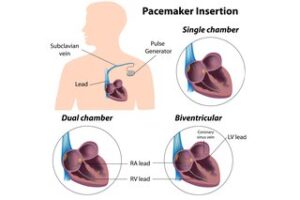
There are several different types of pacemakers.
The main types are:
- single-chamber pacemaker – this has 1 wire, which is connected to either the right atrium (upper heart chamber) or right ventricle (lower heart chamber)
- dual-chamber pacemaker – this has 2 wires, which are connected to the right atrium and right ventricle
- biventricular pacemaker – this has 3 wires, which are connected to the right atrium, right ventricle and left ventricle
There are 4 types of artificial pacemakers:
-
Implantable pulse generators with endocardial or myocardial electrodes
-
External, miniaturized, patient portable, battery-powered, pulse generators with exteriorized electrodes for temporary transvenous endocardial or transthoracic myocardial pacing
-
Console battery or AC-powered cardioverters or monitors with high-current external transcutaneous or low-current endocardial or myocardial circuits for temporary pacing in asynchronous or demand modes, with manual or triggered initiation of pacing
All cardiac pacemakers consist of 2 components: a pulse generator which provides the electrical impulse for myocardial stimulation and 1 or more electrodes or leads which deliver the electrical impulse from the generator to the myocardium. This discussion focuses on the indications of pacemaker placement.
The type of pacemaker you need will depend on your specific heart problem.
Indications:
The most common indications for permanent pacemaker implantation are sinus node dysfunction (SND) and high-grade atrioventricular (AV) block. Guidelines for implantation of cardiac pacemakers have been established by a task force formed jointly by the American College of Cardiology (ACC), the American Heart Association (AHA), and the Heart Rhythm Society (HRS). The European Society of Cardiology has established similar guidelines.
ACC/AHA/HRS divides indications of pacemaker implantation into 3 specific classes:
-
Class I: These are conditions where implantation of a pacemaker is considered necessary and beneficial (benefits much greater than risks).
-
Class II: These are conditions where placement is indicated, but there is conflicting evidence or divergence of opinion. In Class IIa weight of evidence is in favor of efficacy (benefits greater than risk), while in class IIb, the efficacy is less well established (benefits greater than or equal to the risks).
-
Class III: These are conditions in which permanent pacing is not recommended, and in some cases, it may be harmful (risks greater than the benefits).
Complications:
The pacing and CRT are associated with complications. The majority of complications occur in the hospital or during first 6 months. Lead complications are the main reason for the re-implantation of the pacemaker and CRT devices. Other complications include, but are not limited to infections, hematoma formation, pericardial effusion or tamponade, pneumothorax, coronary sinus dissection, or perforation. Some old pacemakers are not MRI safe.
Pacemaker procedures tend to have few complications, which you can discuss with your healthcare provider. In general, the following complications that are possible:
- Allergic reactions: These may happen because of a medication you’re given or you may be allergic to one of the materials used in the pacemaker itself.
- Blood clots: Your healthcare provider may prescribe blood-thinning medications to reduce the risk of developing a blood clot.
- Malfunctions of the pacemaker or its leads: In some cases, a pacemaker lead may get jostled out of position or might break free. Your healthcare provider will recommend limiting your activity for a while after your procedure to avoid this.
- Malfunctions caused by sources outside of your body: Your healthcare provider will give you instructions on devices or machines to avoid so you don’t have pacemaker problems caused by outside electrical interference. Fortunately, advancements in pacemaker technology mean these situations aren’t common.
- Unexpected heart rhythm problems: Some people develop heart rhythm problems — in rare instances — because of the pacemaker. Your healthcare provider can talk to you about these risks and help you avoid them.
Pacemaker implantation has shown a mortality benefit overall.
There are some areas where the indications for a pacemaker are clear, but there are few areas where clinical judgment and expertise plays a greater role. Although the guidelines attempt to define practices that meet the needs of most patients, the ultimate decision for the patient should be based on particular patient presenting scenario, clinician judgment, and discussion with the patient about risks and benefits of the procedure. There are specific pacemaker generators that are used for patients with AV block and sinus node dysfunction depending upon presentation. The different types of generators include a single chamber, dual chamber, and biventricular. A cardiology consult is highly recommended prior to the insertion of a pacemaker.