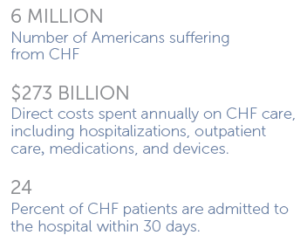
Heart failure (HF) is a syndrome characterized by high prevalence in society, frequent hospitalization, reduced quality of life and high mortality (overall,50% of patients are dead at an interval of 4 years [1], annual mortality varying from 5% to 75%). Outcomes in heart failure are highly variable, prognosis of individual patients differs considerably and trial data, though valuable, does not often give an adequate direction. Taking into account the high prevalence of heart failure in society and its complexity physicians need a model to predict the risk of death, to estimate the survival of heart failure patients. A key element of interest in this area is the survival function, usually noted by S and defined as S(t)=exp(–H0(t)eaTx)=e–H0(t)eaTx
Heart failure–Definition
Heart failure is a syndrome in which structural or functional cardiac conditions impair heart’s ability to supply sufficient blood flow in order to meet the body’s needs, or to do that at an elevated diastolic pressure.
There are many definitions of this complex syndrome, but none is satisfactory, due to the lack of a universally agreed definition and challenges in definitive diagnosis. Until now, only some selective features of this extremely complex physiological state were highlighted in the definitions–oxygen consumption, cardiac pre-load and after-load, left ventricular remodeling and dysfunction, ventricular filling pressures, neuro-hormonal responses, exercise capacity, etc.
The new American and European guidelines and recommendations include new information and have the declared intention to simplify and clarify the previous recommendations.
Heart failure is a clinical syndrome in which patients have featured symptoms typical of heart failure (breathlessness at rest or on exercise, fatigue, tiredness, ankle swelling) and typical signs of heart failure (tachycardia, tachypnoea, pulmonary rales, pleural effusion, raised jugular venous pressure, peripheral edema, hepatomegaly) and objective evidence of a structural or functional abnormality of the heart at rest (cardiomegaly, third heart sound, cardiac murmurs,abnormality on the echocardiogram, raised natriuretic peptide concentration).
A clinical response to a pharmacological therapy directed to heart failure is not sufficient for the diagnosis of heart failure, although the usefulness/efficacy of the treatment may be established by the improvement in symptoms or signs (e.g. diuretic administration).
Heart failure may be classified by structural abnormality (ACC/AHA), or by symptoms relating to functional capacity (NYHA).
ACC/AHA stages of heart failure (based on structure and damage to heart muscle).
-
Stage A: At high risk for developing heart failure. No identified structural or functional abnormality; no signs or symptoms.
-
Stage B: Developed structural heart disease that is strongly associated with the development of heart failure, but without signs or symptoms.
-
Stage C: Symptomatic heart failure associated with underlying structural heart disease.
-
Stage D: Advanced structural heart disease and marked symptoms of heart failure at rest despite maximal medical therapy.
NYHA functional classification (severity based on symptoms and physical activity) (NYHA classification refers to stages C and D)
-
Class Ⅰ:No limitation of physical activity. Ordinary physical activity does not cause fatigue, palpitation, or dyspnoea.
-
Class Ⅱ: Slight limitation of physical activity. Comfortable at rest, but ordinary physical activity results in fatigue, palpitation, or dyspnoea.
-
Class Ⅲ: Marked limitation of physical activity. Comfortable at rest, but less than ordinary activity results in fatigue, palpitation, or dyspnoea.
-
Class Ⅳ: Unable to carry on any physical activity without discomfort. Symptoms at rest. If any physical activity is undertaken, discomfort is increased.